Attention deficit hyperactivity disorder (ADHD)
BASIC INFORMATION
DEFINITION
Attention deficit hyperactivity disorder (ADHD) follows a persistent pattern (lasting at least 6 mo) of inattention or hyperactivity/impulsivity that is greater than expected for age and that begins before age 7 yr. The disorder is further defined by dysfunction in at least two settings (e.g., home, school, day care).
SYNONYMS
Hyperactivity
Attention deficit disorder (ADD)
EPIDEMIOLOGY & DEMOGRAPHICS
PREVALENCE (IN U.S.): 35% of school-age children
PREDOMINANT SEX: Males > females, with rates ranging from 4:1 to 9:1
PREDOMINANT AGE:
• Onset must occur before age 7 yr.
• At least 20% experience spontaneous remissions by adolescence; however, the disorder may persist into adulthood.
PEAK INCIDENCE: Diagnosis is usually made after child begins school (ages 6 to 9 yr).
GENETICS:
• Familial pattern in many patients with ADHD
• Specific thyroid hormone abnormality in a very small fraction of familial ADHD
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Usually diagnosed in elementary school, where achievement is compromised and behavioral dyscontrol is less tolerated
• Wide array of symptoms, including difficulty sustaining attention, frequent careless mistakes, failure to follow instructions, difficulty organizing activities, distractability, forgetfulness, fidgeting, inability to sit still or play quietly, excessive activity or speech, inability to await turn, or intrusiveness
• May exhibit bossiness, stubbornness, demoralization, mood lability, and poor self-esteem
• IQ scores slightly lower than the general population

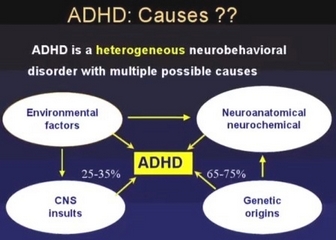
ETIOLOGY
• Probability of multiple etiologies
• Associated and possibly etiologic factors: comorbid Tourette’s, a history of abuse or neglect, lead poisoning, previous encephalitis, drug exposure in utero, low birth weight, and mental retardation. If possible, a specific diagnosis should be made.
• Thyroid hormone metabolism abnormalities identified in a pedigree of familial ADHD
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
• In early childhood, may be difficult to distinguish from normal active children.
• ADHD may overlap symptoms in children with disruptive behavior such as conduct disorder or oppositional defiant disorders.
• School and behavioral problems are associated with a learning disability (these disorders often coexist).
• Bipolar disorder may be confused with ADHD, but it can be distinguished by the episodic nature of bipolar illness and the pervasive presence of ADHD.
WORKUP
• History with collateral information from parents and teachers is central to the diagnosis.
• Neurologic examination including imaging studies is used to uncover nonspecific, nonvocal, soft neurologic signs that frequently can be found in ADHD children.
• Questionnaires for parents and adolescents aid in the diagnosis.
• Psychologic testing is useful to diagnose a learning disability.
TREATMENT
NONPHARMACOLOGIC THERAPY
Children generally do better in special education settings with behavioral management of the disruptive behavior.
ACUTE GENERAL Rx
• Stimulants: mainstay of treating ADHD; include methylphenidate (Ritalin), dextroamphetamine (Dexedrine), and pemoline (Cylert; may cause rare, severe
hepatotoxicity))
• The amphetamine-dextroamphetamine combination Adderall is also useful in children with ADHD. Once-daily Adderall is as effective as twice-daily
methylphenidate and both are superior to once-daily methylphenidate.
• Atomoxetine (strattera), a selective norepinephrine reuptake inhibitor was recently approved for treatment of ADHD.
• Adjuncts: tricyclic antidepressants (rare cardiac deaths in children and adolescents warrant caution); serotonin reuptake-inhibiting antidepressants, bupropion
(safer but efficacy not as well documented), clonidine, and neuroleptics
DISPOSITION
• Severity generally decreases with age.
• In late adolescence, the symptom severity is quite mild in many individuals.
• Full or partial aspects of the disorder are possibly persistent into mid-adulthood and require ongoing pharmacotherapy.
REFERRAL
• If diagnosis is complicated by coexisting conditions
• If treatment with stimulants is not adequately effective
• Probability of multiple etiologies
• Associated and possibly etiologic factors: comorbid Tourette’s, a history of abuse or neglect, lead poisoning, previous encephalitis, drug exposure in utero, low birth weight, and mental retardation. If possible, a specific diagnosis should be made.
• Thyroid hormone metabolism abnormalities identified in a pedigree of familial ADHD
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
• In early childhood, may be difficult to distinguish from normal active children.
• ADHD may overlap symptoms in children with disruptive behavior such as conduct disorder or oppositional defiant disorders.
• School and behavioral problems are associated with a learning disability (these disorders often coexist).
• Bipolar disorder may be confused with ADHD, but it can be distinguished by the episodic nature of bipolar illness and the pervasive presence of ADHD.
WORKUP
• History with collateral information from parents and teachers is central to the diagnosis.
• Neurologic examination including imaging studies is used to uncover nonspecific, nonvocal, soft neurologic signs that frequently can be found in ADHD children.
• Questionnaires for parents and adolescents aid in the diagnosis.
• Psychologic testing is useful to diagnose a learning disability.
TREATMENT
NONPHARMACOLOGIC THERAPY
Children generally do better in special education settings with behavioral management of the disruptive behavior.
ACUTE GENERAL Rx
• Stimulants: mainstay of treating ADHD; include methylphenidate (Ritalin), dextroamphetamine (Dexedrine), and pemoline (Cylert; may cause rare, severe
hepatotoxicity))
• The amphetamine-dextroamphetamine combination Adderall is also useful in children with ADHD. Once-daily Adderall is as effective as twice-daily
methylphenidate and both are superior to once-daily methylphenidate.
• Atomoxetine (strattera), a selective norepinephrine reuptake inhibitor was recently approved for treatment of ADHD.
• Adjuncts: tricyclic antidepressants (rare cardiac deaths in children and adolescents warrant caution); serotonin reuptake-inhibiting antidepressants, bupropion
(safer but efficacy not as well documented), clonidine, and neuroleptics
DISPOSITION
• Severity generally decreases with age.
• In late adolescence, the symptom severity is quite mild in many individuals.
• Full or partial aspects of the disorder are possibly persistent into mid-adulthood and require ongoing pharmacotherapy.
REFERRAL
• If diagnosis is complicated by coexisting conditions
• If treatment with stimulants is not adequately effective

Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!