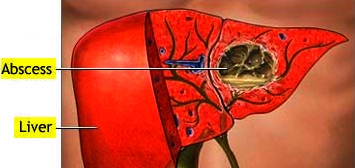
Abscess, liver
BASIC INFORMATION
Liver abscess is a necrotic infection of the liver usually classified as pyogenic or amebic.
SYNONYMS
Pyogenic hepatic abscess, Amebic hepatic abscess
EPIDEMIOLOGY & DEMOGRAPHICS
• Worldwide, amebic liver abscess is more common than pyogenic liver abscess.
• In the U.S., pyogenic liver abscess is more common than amebic liver abscess.
• Incidence of pyogenic liver abscess is 6 to 10 cases per 100,000.
• Amebic liver abscesses complicate amebic colitis in nearly 10% of cases.
• Most abscesses occur on the right lobe of the liver.
• More common in men than women.
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Fever, chills, and sweats
• Anorexia with weight loss
• Nausea, vomiting, and diarrhea
• Cough with pleuritic chest pain
• Right upper quadrant abdominal pain
• Hepatomegaly
• Splenomegaly
• Jaundice
• Pleural effusions, rales, and friction rubs may be present.
ETIOLOGY
• Pyogenic liver abscess is usually polymicrobial (E. coli, K. pneumoniae, P. aeruginosa, Proteus, Bacteroides, Fusobacterium, Actinomyces, grampositive anaerobes and S. aureus).
• Amebic hepatic abscess is caused by the parasite Entamoeba histolytica.
• Pyogenic liver abscess occurs from:
1. Biliary disease with cholangitis
2. Gallbladder disease with contiguous spread to the liver
3. Diverticulitis or appendicitis with spread via the portal circulation
4. Hematogenous spread via the hepatic artery
5. Penetrating wounds
6. Cryptogenic
• Amebiasis is usually due to fecal-oral contamination and invades the intestinal mucosa gaining entry into the portal system to reach the liver.
• Incidence of pyogenic liver abscess is 6 to 10 cases per 100,000.
• Amebic liver abscesses complicate amebic colitis in nearly 10% of cases.
• Most abscesses occur on the right lobe of the liver.
• More common in men than women.
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Fever, chills, and sweats
• Anorexia with weight loss
• Nausea, vomiting, and diarrhea
• Cough with pleuritic chest pain
• Right upper quadrant abdominal pain
• Hepatomegaly
• Splenomegaly
• Jaundice
• Pleural effusions, rales, and friction rubs may be present.
ETIOLOGY
• Pyogenic liver abscess is usually polymicrobial (E. coli, K. pneumoniae, P. aeruginosa, Proteus, Bacteroides, Fusobacterium, Actinomyces, grampositive anaerobes and S. aureus).
• Amebic hepatic abscess is caused by the parasite Entamoeba histolytica.
• Pyogenic liver abscess occurs from:
1. Biliary disease with cholangitis
2. Gallbladder disease with contiguous spread to the liver
3. Diverticulitis or appendicitis with spread via the portal circulation
4. Hematogenous spread via the hepatic artery
5. Penetrating wounds
6. Cryptogenic
• Amebiasis is usually due to fecal-oral contamination and invades the intestinal mucosa gaining entry into the portal system to reach the liver.
DIAGNOSIS
The diagnosis of liver abscess requires a high index of suspicion after a detailed history and physical examination. Imaging studies confirm the presence of a liver abscess.
The diagnosis of liver abscess requires a high index of suspicion after a detailed history and physical examination. Imaging studies confirm the presence of a liver abscess.
DIFFERENTIAL DIAGNOSIS
• Cholangitis
• Cholecystitis
• Diverticulitis
• Appendicitis
• Perforated viscus
• Mesentery ischemia
• Pulmonary embolism
• Pancreatitis
WORKUP
• The workup of a liver abscess should focus on differentiating between amebic and pyogenic causes.
• Features suggesting an amebic cause are: travel to an endemic area, single abscess rather than multiple abscesses, subacute onset of symptoms, and absence
of conditions predisposing to pyogenic liver abscess as highlighted under “Etiology.”
• Laboratory studies are not specific but useful as adjunctive tests.
• Imaging studies cannot differentiate between the two, and bacteriologic cultures may be sterile in 50% of the cases.
LABORATORY TESTS
• CBC showing leukocytosis
• Liver function tests: alkaline phosphatase is most commonly elevated (95%); AST and ALT elevated in 50% of cases
• PT (INR) prolonged (70%)
• Blood cultures positive in 50% of cases
• Aspiration (50% sterile)
• Stool samples for E. histolytica trophozoites (positive in 10% to 15% of amebic liver abscess cases)
• Serologic testing for E. histolytica does not differentiate acute from old infections
TREATMENT
NONPHARMACOLOGIC THERAPY
• The management of pyogenic liver abscess differs from that of amebic liver abscess.
• Medical management is the cornerstone of therapy in amebic liver abscess, whereas early intervention in the form of surgical therapy or catheter drainage and
parenteral antibiotics is the rule in pyogenic liver abscess.
ACUTE GENERAL Rx
• Percutaneous drainage under CT or ultrasound guidance is essential in the treatment of pyogenic liver abscesses.
• Aspiration of hepatic amebic abscesses is not required unless there is no response to treatment or a pyogenic cause is being considered.
• Antibiotic treatment for pyogenic liver abscess initially is empirical triple therapy with penicillin, aminoglycoside, and metronidazole.
1. Parenteral antibiotics are continued for 2 wk and followed by 4 to 6 wk PO therapy.
2. Clindamycin with an aminoglycoside or imipenem alone are alternative choices.
• Antibiotic coverage for amebic liver abscesses include:
1. Metronidazole 750 mg PO tid for 10 days
2. Dehydroemetine 1 mg/kg/day IM for 5 days followed by chloroquine 1 g/day for 2 days; then 500 mg/day for 2 to 3 wk can be used as an alternative to metronidazole
CHRONIC Rx
If fever persists for 2 wk despite percutaneous drainage and antibiotic therapy as outlined under “Acute General Rx,” surgery is indicated.
DISPOSITION
• Most patients with pyogenic liver abscesses defervesce within 2 wk of treatment with antibiotics and drainage.
• Pyogenic liver abscess cure rates using percutaneous drainage and antibiotics have been reported to be between 88% and 100%.
• Mortality of untreated pyogenic liver abscess is nearly 100%.
• Most patients with amebic liver abscesses defervesce within 4 to 5 days of treatment.
• Amebic liver abscess mortality rate is <1% unless complications occur.
• Cholangitis
• Cholecystitis
• Diverticulitis
• Appendicitis
• Perforated viscus
• Mesentery ischemia
• Pulmonary embolism
• Pancreatitis
WORKUP
• The workup of a liver abscess should focus on differentiating between amebic and pyogenic causes.
• Features suggesting an amebic cause are: travel to an endemic area, single abscess rather than multiple abscesses, subacute onset of symptoms, and absence
of conditions predisposing to pyogenic liver abscess as highlighted under “Etiology.”
• Laboratory studies are not specific but useful as adjunctive tests.
• Imaging studies cannot differentiate between the two, and bacteriologic cultures may be sterile in 50% of the cases.
LABORATORY TESTS
• CBC showing leukocytosis
• Liver function tests: alkaline phosphatase is most commonly elevated (95%); AST and ALT elevated in 50% of cases
• PT (INR) prolonged (70%)
• Blood cultures positive in 50% of cases
• Aspiration (50% sterile)
• Stool samples for E. histolytica trophozoites (positive in 10% to 15% of amebic liver abscess cases)
• Serologic testing for E. histolytica does not differentiate acute from old infections
TREATMENT
NONPHARMACOLOGIC THERAPY
• The management of pyogenic liver abscess differs from that of amebic liver abscess.
• Medical management is the cornerstone of therapy in amebic liver abscess, whereas early intervention in the form of surgical therapy or catheter drainage and
parenteral antibiotics is the rule in pyogenic liver abscess.
ACUTE GENERAL Rx
• Percutaneous drainage under CT or ultrasound guidance is essential in the treatment of pyogenic liver abscesses.
• Aspiration of hepatic amebic abscesses is not required unless there is no response to treatment or a pyogenic cause is being considered.
• Antibiotic treatment for pyogenic liver abscess initially is empirical triple therapy with penicillin, aminoglycoside, and metronidazole.
1. Parenteral antibiotics are continued for 2 wk and followed by 4 to 6 wk PO therapy.
2. Clindamycin with an aminoglycoside or imipenem alone are alternative choices.
• Antibiotic coverage for amebic liver abscesses include:
1. Metronidazole 750 mg PO tid for 10 days
2. Dehydroemetine 1 mg/kg/day IM for 5 days followed by chloroquine 1 g/day for 2 days; then 500 mg/day for 2 to 3 wk can be used as an alternative to metronidazole
CHRONIC Rx
If fever persists for 2 wk despite percutaneous drainage and antibiotic therapy as outlined under “Acute General Rx,” surgery is indicated.
DISPOSITION
• Most patients with pyogenic liver abscesses defervesce within 2 wk of treatment with antibiotics and drainage.
• Pyogenic liver abscess cure rates using percutaneous drainage and antibiotics have been reported to be between 88% and 100%.
• Mortality of untreated pyogenic liver abscess is nearly 100%.
• Most patients with amebic liver abscesses defervesce within 4 to 5 days of treatment.
• Amebic liver abscess mortality rate is <1% unless complications occur.
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!
