Anatomy of Blood Vessels
Blood vessels are of three types: arteries, capillaries, and veins (Fig. 12.10). These vessels function to:
1. transport blood and its contents;
2. carry out exchange of gases in the pulmonary capillaries and exchange of gases plus nutrients for waste at the systemic capillaries;
3. regulate blood pressure;
4. direct blood flow to those systemic tissues that most require it at the moment.
Arteries and Arterioles
Arteries (Fig. 12.10a) transport blood away from the heart. They have thick, strong walls composed of three layers: (1) The tunica interna is an endothelium layer with a basement membrane. (2) The tunica media is a thick middle layer of smooth muscle and elastic fibers. (3) The tunica externa is an outer connective tissue layer composed principally of elastic and collagen fibers. Arterial walls are sometimes so thick that they are supplied with blood vessels. The radius of an artery allows the blood to flow rapidly and the elasticity of an artery allows it to expand when the heart contracts and recoil when the heart rests. This means that blood continues to flow in an artery even when the heart is in diastole.
Arterioles are small arteries just visible to the naked eye. The middle layer of these vessels has some elastic tissue but is composed mostly of smooth muscle whose fibers encircle the arteriole. If the muscle fibers contract, the lumen (cavity) of the arteriole decreases; if the fibers relax, the lumen of the arteriole enlarges. Whether arterioles are constricted or dilated affects blood distribution and blood pressure. When a muscle is actively contracting, for example, the arterioles in the vicinity dilate so that the needs of the muscle for oxygen and glucose are met. As we shall see, the autonomic nervous system helps control blood pressure by regulating the number of arterioles that are contracted. The greater the number of vessels contracted, the higher the resistance to blood flow, and hence, the higher the blood pressure. The greater the number of vessels dilated, the lower the resistance to blood flow, and hence, the lower the blood pressure.
Arteriosclerosis
The plaques associated with atherosclerosis lead to the deposition of calcium salts and the formation of nonelastic scar tissue, resulting in increased rigidity of the vessel wall. This process of hardening of the arteries, or arteriosclerosis, not only contributes to hypertension but also increases the risk of a heart attack or stroke.
Arterioles branch into capillaries (Fig. 12.10b), which are extremely narrow, microscopic blood vessels with a wall composed of only one layer of endothelial cells. Capillary beds (networks of many capillaries) are present in all regions of the body; consequently, a cut in any body tissue draws blood. Capillaries are an important part of the cardiovascular system because nutrient and waste molecules are exchanged only across their thin walls. Oxygen and glucose diffuse out of capillaries into the tissue fluid that surrounds cells, and carbon dioxide and other wastes diffuse into the capillaries. Because capillaries serve the needs of the cells, the heart and other vessels of the cardiovascular system can be considered a means by which blood is conducted to and from the capillaries.
Not all capillary beds are open or in use at the same time. For instance, after a meal, the capillary beds of the digestive tract are usually open, and during muscular exercise, the capillary beds of the skeletal muscles are open.
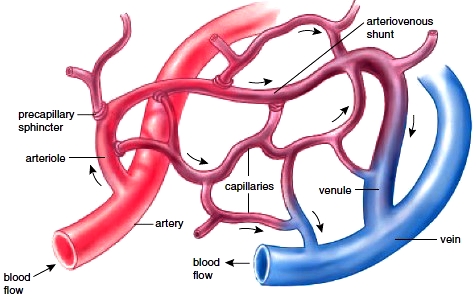
Most capillary beds have a shunt that allows blood to move directly from an arteriole to a venule (a small vessel leading to a vein) when the capillary bed is closed. Sphincter muscles, called precapillary sphincters, encircle the entrance to each capillary (Fig. 12.11). When the capillary bed is closed, the capillary sphincters are constricted, preventing blood from entering the capillaries; when the capillary bed is open, the capillary sphincters are relaxed. As would be expected, the larger the number of capillary beds open, the lower the blood pressure.
Veins and smaller vessels called venules carry blood from the capillary beds to the heart. The venules first drain the blood from the capillaries and then join together to form a vein. The wall of a vein is much thinner than that of an artery because the middle layer of muscle and elastic fibers is thinner (see Fig. 12.10c). Within some veins, especially the major veins of the arms and legs, valves allow blood to flow only toward the heart when they are open and prevent the backward flow of blood when they are closed.
At any given time, more than half of the total blood volume is found in the veins and venules. If blood is lost due to, for example, hemorrhaging, sympathetic nervous stimulation causes the veins to constrict, providing more blood to the rest of the body. In this way, the veins act as a blood reservoir.
Varicose Veins and Phlebitis
Varicose veins are abnormal and irregular dilations in superficial (near the surface) veins, particularly those in the lower legs. Varicose veins in the rectum, however, are commonly called piles, or more properly, hemorrhoids. Varicose veins develop when the valves of the veins become weak and ineffective due to backward pressure of the blood.
Phlebitis, or inflammation of a vein, is a more serious condition because thromboembolism can occur. In this instance, the embolus may eventually come to rest in a pulmonary arteriole, blocking circulation through the lungs. This condition, termed pulmonary embolism, can result in death.
Arteriosclerosis
The plaques associated with atherosclerosis lead to the deposition of calcium salts and the formation of nonelastic scar tissue, resulting in increased rigidity of the vessel wall. This process of hardening of the arteries, or arteriosclerosis, not only contributes to hypertension but also increases the risk of a heart attack or stroke.
Capillaries
Arterioles branch into capillaries (Fig. 12.10b), which are extremely narrow, microscopic blood vessels with a wall composed of only one layer of endothelial cells. Capillary beds (networks of many capillaries) are present in all regions of the body; consequently, a cut in any body tissue draws blood. Capillaries are an important part of the cardiovascular system because nutrient and waste molecules are exchanged only across their thin walls. Oxygen and glucose diffuse out of capillaries into the tissue fluid that surrounds cells, and carbon dioxide and other wastes diffuse into the capillaries. Because capillaries serve the needs of the cells, the heart and other vessels of the cardiovascular system can be considered a means by which blood is conducted to and from the capillaries.
Not all capillary beds are open or in use at the same time. For instance, after a meal, the capillary beds of the digestive tract are usually open, and during muscular exercise, the capillary beds of the skeletal muscles are open.
Most capillary beds have a shunt that allows blood to move directly from an arteriole to a venule (a small vessel leading to a vein) when the capillary bed is closed. Sphincter muscles, called precapillary sphincters, encircle the entrance to each capillary (Fig. 12.11). When the capillary bed is closed, the capillary sphincters are constricted, preventing blood from entering the capillaries; when the capillary bed is open, the capillary sphincters are relaxed. As would be expected, the larger the number of capillary beds open, the lower the blood pressure.
Veins and Venules
Veins and smaller vessels called venules carry blood from the capillary beds to the heart. The venules first drain the blood from the capillaries and then join together to form a vein. The wall of a vein is much thinner than that of an artery because the middle layer of muscle and elastic fibers is thinner (see Fig. 12.10c). Within some veins, especially the major veins of the arms and legs, valves allow blood to flow only toward the heart when they are open and prevent the backward flow of blood when they are closed.
At any given time, more than half of the total blood volume is found in the veins and venules. If blood is lost due to, for example, hemorrhaging, sympathetic nervous stimulation causes the veins to constrict, providing more blood to the rest of the body. In this way, the veins act as a blood reservoir.
Varicose Veins and Phlebitis
Varicose veins are abnormal and irregular dilations in superficial (near the surface) veins, particularly those in the lower legs. Varicose veins in the rectum, however, are commonly called piles, or more properly, hemorrhoids. Varicose veins develop when the valves of the veins become weak and ineffective due to backward pressure of the blood.
Phlebitis, or inflammation of a vein, is a more serious condition because thromboembolism can occur. In this instance, the embolus may eventually come to rest in a pulmonary arteriole, blocking circulation through the lungs. This condition, termed pulmonary embolism, can result in death.

Figure 12.10 Blood vessels. The walls of arteries and veins have three layers. The tunica interna is an endothelium with a basement membrane; the tunica media is smooth muscle tissue and elastic fibers; the tunica externa is composed of connective tissue. a. Arteries have a thicker wall than veins because they have a thicker middle layer than veins. b. Capillary walls are one-cell-thick endothelium. c. Veins are larger in diameter than arteries, so collectively, veins have a larger holding capacity than arteries.
Figure 12.11 Anatomy of a capillary bed. A capillary bed forms a maze of capillary vessels that lies between an arteriole and a venule. When sphincter muscles are relaxed, the capillary bed is open, and blood flows through the capillaries. When sphincter muscles are contracted, blood flows through a shunt that carries blood directly from an arteriole to a venule. As blood passes through a capillary in the tissues, it gives up its oxygen (O2). Therefore, blood goes from being O2-rich in the arteriole (red color) to being O2-poor in the vein (blue color).
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!