TREATMENT
All fractures: elevation and ice to control swelling for 48 to 72 hr.
ACUTE GENERAL Rx
• Clinical and roentgenographic assessment of the status of the ankle mortise and stability of the injury is mandatory to determine treatment.
• There is potential for displacement if both sides of the joint are significantly injured (e.g., fracture of the lateral malleolus with deltoid ligament injury).
• Deviation of the position of the talus in the mortise could lead to traumatic arthritis.
• If there is no widening of the ankle mortise, many injuries can be safely treated with simple casting without reduction:
1. Undisplaced or avulsion fractures of either malleolus below the ankle joint line:
a. Stability of the joint is not compromised and a short leg walking cast or ankle support is sufficient.
b. Weight bearing is allowed as tolerated.
c. In 4 to 6 wk, protection may be discontinued.
2. Isolated undisplaced fractures of the medial, lateral, or posterior malleolus:
a. Usually stable and require only the application of a short leg walking cast with the ankle in the neutral position or fracture cast boot.
b. Immobilization should be continued for 8 wk.
c. Fracture line of lateral malleolus may persist roentgenographically for several months, but immobilization beyond 8 wk is usually unnecessary.
d. Undisplaced bimalleolar fractures are treated with a long leg cast flexed 30° at the knee to prevent motion and displacement of the fracture fragments. In 4 wk, a short leg walking cast may be applied for an additional 4 wk.
3. Isolated fractures of the lateral malleolus that are slightly displaced:
a. May be treated with casting if no medial injury is present.
b. A below-knee walking cast is applied with ankle in the neutral position and weight bearing is allowed as tolerated.
c. Six weeks of immobilization is sufficient.
d. If medial tenderness is present, suggesting deltoid ligament rupture, a carefully molded cast may suffice if weight bearing is not allowed and the patient is followed closely for signs of instability, especially after swelling recedes. If significant widening of the medial ankle mortise (increase in the “medial clear space”) develops as a result of lateral displacement of the talus, referral for possible reduction is indicated.
e. If signs of instability are already present at initial examination (widening of the medial clear space with medial tenderness), referral is indicated.
4. Undisplaced fracture of the distal fibular epiphysis:
a. Diagnosed clinically.
b. There is tenderness over the epiphyseal plate.
c. Roentgenographic findings are often negative.
All fractures: elevation and ice to control swelling for 48 to 72 hr.
ACUTE GENERAL Rx
• Clinical and roentgenographic assessment of the status of the ankle mortise and stability of the injury is mandatory to determine treatment.
• There is potential for displacement if both sides of the joint are significantly injured (e.g., fracture of the lateral malleolus with deltoid ligament injury).
• Deviation of the position of the talus in the mortise could lead to traumatic arthritis.
• If there is no widening of the ankle mortise, many injuries can be safely treated with simple casting without reduction:
1. Undisplaced or avulsion fractures of either malleolus below the ankle joint line:
a. Stability of the joint is not compromised and a short leg walking cast or ankle support is sufficient.
b. Weight bearing is allowed as tolerated.
c. In 4 to 6 wk, protection may be discontinued.
2. Isolated undisplaced fractures of the medial, lateral, or posterior malleolus:
a. Usually stable and require only the application of a short leg walking cast with the ankle in the neutral position or fracture cast boot.
b. Immobilization should be continued for 8 wk.
c. Fracture line of lateral malleolus may persist roentgenographically for several months, but immobilization beyond 8 wk is usually unnecessary.
d. Undisplaced bimalleolar fractures are treated with a long leg cast flexed 30° at the knee to prevent motion and displacement of the fracture fragments. In 4 wk, a short leg walking cast may be applied for an additional 4 wk.
3. Isolated fractures of the lateral malleolus that are slightly displaced:
a. May be treated with casting if no medial injury is present.
b. A below-knee walking cast is applied with ankle in the neutral position and weight bearing is allowed as tolerated.
c. Six weeks of immobilization is sufficient.
d. If medial tenderness is present, suggesting deltoid ligament rupture, a carefully molded cast may suffice if weight bearing is not allowed and the patient is followed closely for signs of instability, especially after swelling recedes. If significant widening of the medial ankle mortise (increase in the “medial clear space”) develops as a result of lateral displacement of the talus, referral for possible reduction is indicated.
e. If signs of instability are already present at initial examination (widening of the medial clear space with medial tenderness), referral is indicated.
4. Undisplaced fracture of the distal fibular epiphysis:
a. Diagnosed clinically.
b. There is tenderness over the epiphyseal plate.
c. Roentgenographic findings are often negative.
Ankle fracture
BASIC INFORMATION
Ankle fractures involve the lateral, medial, or posterior malleolus of the ankle and may occur either alone or in some combination. Associated ligamentous injuries are included.
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Deformity usually dependent on extent of displacement
• Pain, tenderness, and hemorrhage at the site of injury
• Gentle palpation of ligamentous structures (especially deltoid ligament) to determine the extent of soft tissue injury
• Evaluation of distal neurovascular status; results recorded
ETIOLOGY
• The ankle depends on its ligamentous and bony support for stability. The joint, or mortise, is an inverted U with the dome of the talus fitting into the medial and lateral malleoli. The posterior margin of the tibia is often called the third or posterior malleolus.
• Most common ankle fractures are the result of eversion or lateral rotation forces on the talus (in contrast to common sprains, which are caused usually by inversion).
DIAGNOSIS
IMAGING STUDIES
Standard AP and lateral views accompanied by an AP taken 15° internally rotated. The last view is taken to properly visualize the mortise.
IMAGING STUDIES
Standard AP and lateral views accompanied by an AP taken 15° internally rotated. The last view is taken to properly visualize the mortise.


Bones of the right foot.
Ankle fracture
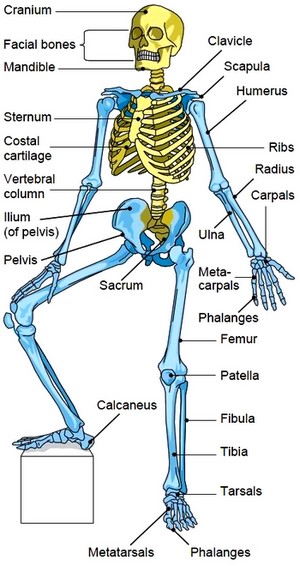
The skeleton. The axial skeleton is shown in yellow; the appendicular, in blue.
d. A short leg walking cast is applied for 4 wk.
e. Growth disturbance is rare.
5. Isolated posterior malleolar fractures involving less than 25% of the joint surface on the lateral roentgeno-gram:
Safely treated by applying a short leg walking cast or fracture brace. (Fractures involving >25% of the weight-bearing surface should be referred because of the potential for instability and subsequent traumatic arthritis)
CHRONIC Rx
• Early motion is encouraged through a home exercise program.
• Protection from reinjury is appropriate for 4 to 6 wk following cast or brace removal.
• Temporary increase in lower extremity swelling that frequently occurs after short leg cast removal may benefit from the use of support hose.
DISPOSITION
Significant factors involved in the development of traumatic arthritis:
• Amount of joint trauma at the time of injury
• Eventual position of the talus in the mortise
Fracture nonunion is uncommon unless displacement is significant.
REFERRAL
Orthopedic consultation for:
• Unstable ankle joint
• Widened ankle mortise
• Posterior malleolar fracture over 25% of joint with incongruity
• Marked displacement of fracture fragment
e. Growth disturbance is rare.
5. Isolated posterior malleolar fractures involving less than 25% of the joint surface on the lateral roentgeno-gram:
Safely treated by applying a short leg walking cast or fracture brace. (Fractures involving >25% of the weight-bearing surface should be referred because of the potential for instability and subsequent traumatic arthritis)
CHRONIC Rx
• Early motion is encouraged through a home exercise program.
• Protection from reinjury is appropriate for 4 to 6 wk following cast or brace removal.
• Temporary increase in lower extremity swelling that frequently occurs after short leg cast removal may benefit from the use of support hose.
DISPOSITION
Significant factors involved in the development of traumatic arthritis:
• Amount of joint trauma at the time of injury
• Eventual position of the talus in the mortise
Fracture nonunion is uncommon unless displacement is significant.
REFERRAL
Orthopedic consultation for:
• Unstable ankle joint
• Widened ankle mortise
• Posterior malleolar fracture over 25% of joint with incongruity
• Marked displacement of fracture fragment
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!