Aseptic necrosis
BASIC INFORMATION
DEFINITION
Cell death in components of bone: hematopoietic fat marrow and mineralized tissue.
SYNONYMS
Osteonecrosis, Avascular Necrosis
Avascular (Aseptic) Necrosis of the Femoral Head.
The etiology cannot be determined in every case, but common causes of this problem include high-dose glucocorticoid therapy, alcohol abuse, hepatic and pancreatic diseases, metabolic disorders, such as hyperlipidemia, Gaucher disease, renal osteopathy, and hyperuricemia, rheumatoid arthritis and other collagenoses, coagulopathies, hemoglobinopathies (sickle cell anemia), and decompression trauma (in professional and sport divers).Radiologic signs include subchondral flattening of the femoral head, subchondral radiolucency, and fragmentation. The differential diagnosis of avascular necrosis of the femoral head in adults includes monoarthritis, bone destruction by tumor, transient osteoporosis of the femoral head, and infection.
Osteonecrosis of the Knee Joint (Ahlback Disease). This disorder consists of spontaneous, idiopathic osteonecrosis of the knee joint, usually arising between the ages of 40 and 60 and affecting women three times more often than men. Pain in the knee joint usually begins acutely. Physical examination typically reveals tenderness to pressure on the affected femoral or tibial condyle. There may be an accompanying synovitis with joint effusion.
Osteonecrosis can also arise in the aftermath of an arthroscopic procedure or any other type of knee trauma. Patients with persistent discomfort after arthroscopy should therefore undergo an MRI study of the knee to rule out incipient or established osteonecrosis.
The differential diagnosis of Ahlback disease includes osteochondritis dissecans, an activated arthrosis, meniscus lesions, stress fractures, and transient osteoporosis. Osteochondritis dissecans and activated arthrosis usually cause pain of gradually increasing severity. The clinical differentiation of a meniscus lesion from osteonecrosis may be more difficult, but MRI often helps in such cases. Transient regional osteoporosis can also cause pain of acute onset.
The differential diagnosis of Ahlback disease includes osteochondritis dissecans, an activated arthrosis, meniscus lesions, stress fractures, and transient osteoporosis. Osteochondritis dissecans and activated arthrosis usually cause pain of gradually increasing severity. The clinical differentiation of a meniscus lesion from osteonecrosis may be more difficult, but MRI often helps in such cases. Transient regional osteoporosis can also cause pain of acute onset.

Table 11 Diseases and other factors in the pathogenesis of osteonecrosis
EPIDEMIOLOGY & DEMOGRAPHICS
• 15,000 new cases per year in the U.S.
• Associated conditions:
1. Corticosteroid treatment: 35%
2. Alcohol abuse: 22%
3. Idiopathic and other: 43%
• Common sites involved
1. Femoral head
2. Femoral condyle
3. Humeral head
4. Navicular and lunate wrist bones
5. Talus
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• May be asymptomatic
• Pain in the involved area exacerbated by movement or weight bearing.
• Decreased range of motion as the disease progresses
• Functional limitation
ETIOLOGY
Final common pathway of conditions that lead to impairment of the blood supply to the involved bone.
• 15,000 new cases per year in the U.S.
• Associated conditions:
1. Corticosteroid treatment: 35%
2. Alcohol abuse: 22%
3. Idiopathic and other: 43%
• Common sites involved
1. Femoral head
2. Femoral condyle
3. Humeral head
4. Navicular and lunate wrist bones
5. Talus
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• May be asymptomatic
• Pain in the involved area exacerbated by movement or weight bearing.
• Decreased range of motion as the disease progresses
• Functional limitation
ETIOLOGY
Final common pathway of conditions that lead to impairment of the blood supply to the involved bone.
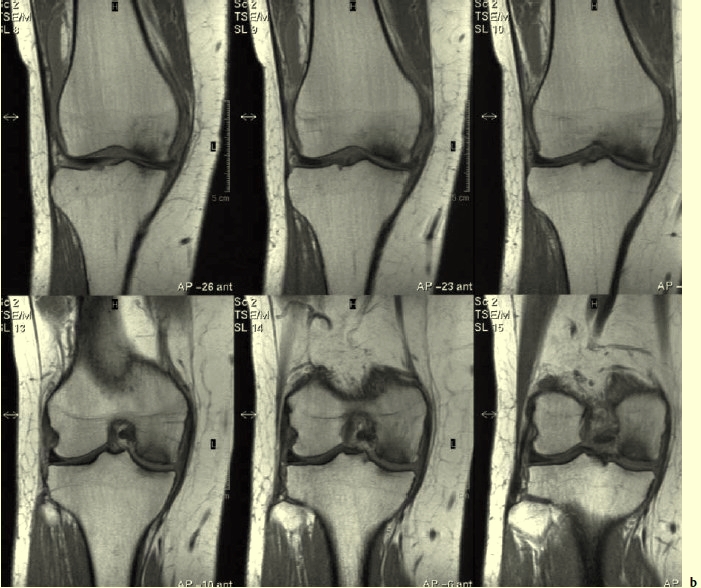
Fig. 11.1 Osteonecrosis of the medial femoral condyle. b MRI.
Stages:
Stage 0
• Asymptomatic
• Normal imaging
• Histologic findings only (i.e., silent osteonecrosis)
Stage 1
• Asymptormatic or symptomatic
• Normal x-ray and CT scan
• Abnormal bone scan and/or MRI
Stage 2
• Abnormal x-rays and/or CT scan including linear sclerosis, focal bead mineralization, cysts; however, the overall architecture of the involved bone is normal
Stage 3
• Early evidence of mechanical bone failure (subchondral fracture), but the overall shape of the bone is still intact
Stage 4
• Flattening or collapse of the bone
Stage 5
• Joint space narrowing
Stage 6
• Extensive joint destruction
DIFFERENTIAL DIAGNOSIS
• None in late stages
• Early: any condition causing focal musculoskeletal pain including arthritis, bursitis, tendinitis, myopathy, neoplastic bone and joint diseases, traumatic injuries, pathologic fractures.
IMAGING STUDIES
1. X-ray: insensitive early in the course. The earliest changes include diffuse ostopenia, areas of radiolucency with sclerotic border, and linear sclerosis. Later a
subchondral lucency (crescent sign) indicates subchondral fracture. More advanced cases reveal flattening, collapsed bone and abnormal bone contour. In late
disease, osteoarthritic changes are seen:
2. Bone scan:
• Early: “cold” area
• Later: increased radionuclide uptake as a result of remodeling
• Sensitivity in early disease is only 70% and specificity is poor
3. CT scan: may reveal central necrosis and area of collapse before those are visible in xray.
4. MRI: the most sensitive technology to diagnose early aseptic necrosis. The first sign is a margin of low signal. An inner border of high signal associated with a low-signal line is specific of aseptic necrosis (“double line sign”). Sensitivity is 75%-100%.
TREATMENT
PREVENTION
• Management of etiologic conditions
• Minimize corticosteroid use
MEDICAL TREATMENT
• Decrease weight bearing of affected area
• Pulsing electromagnetic fields applied externally (still experimental)
• Peripheral vasodilators (e.g., dihydrogotamine) (unproven)
SURGICAL TREATMENT
• Core decompression: effectiveness 35%-95% in early phases
• Bone grafting
• Osteotomies
• Joint replacement
PROGNOSIS
• When diagnosed at an early stage treatment is appropriate in all cases because 85%-90% can be expected to progress to a more advanced stage
• Contralateral joint involvement is common (30%-70%)
Stage 0
• Asymptomatic
• Normal imaging
• Histologic findings only (i.e., silent osteonecrosis)
Stage 1
• Asymptormatic or symptomatic
• Normal x-ray and CT scan
• Abnormal bone scan and/or MRI
Stage 2
• Abnormal x-rays and/or CT scan including linear sclerosis, focal bead mineralization, cysts; however, the overall architecture of the involved bone is normal
Stage 3
• Early evidence of mechanical bone failure (subchondral fracture), but the overall shape of the bone is still intact
Stage 4
• Flattening or collapse of the bone
Stage 5
• Joint space narrowing
Stage 6
• Extensive joint destruction
DIFFERENTIAL DIAGNOSIS
• None in late stages
• Early: any condition causing focal musculoskeletal pain including arthritis, bursitis, tendinitis, myopathy, neoplastic bone and joint diseases, traumatic injuries, pathologic fractures.
IMAGING STUDIES
1. X-ray: insensitive early in the course. The earliest changes include diffuse ostopenia, areas of radiolucency with sclerotic border, and linear sclerosis. Later a
subchondral lucency (crescent sign) indicates subchondral fracture. More advanced cases reveal flattening, collapsed bone and abnormal bone contour. In late
disease, osteoarthritic changes are seen:
2. Bone scan:
• Early: “cold” area
• Later: increased radionuclide uptake as a result of remodeling
• Sensitivity in early disease is only 70% and specificity is poor
3. CT scan: may reveal central necrosis and area of collapse before those are visible in xray.
4. MRI: the most sensitive technology to diagnose early aseptic necrosis. The first sign is a margin of low signal. An inner border of high signal associated with a low-signal line is specific of aseptic necrosis (“double line sign”). Sensitivity is 75%-100%.
TREATMENT
PREVENTION
• Management of etiologic conditions
• Minimize corticosteroid use
MEDICAL TREATMENT
• Decrease weight bearing of affected area
• Pulsing electromagnetic fields applied externally (still experimental)
• Peripheral vasodilators (e.g., dihydrogotamine) (unproven)
SURGICAL TREATMENT
• Core decompression: effectiveness 35%-95% in early phases
• Bone grafting
• Osteotomies
• Joint replacement
PROGNOSIS
• When diagnosed at an early stage treatment is appropriate in all cases because 85%-90% can be expected to progress to a more advanced stage
• Contralateral joint involvement is common (30%-70%)
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!