
WORKUP
• ECG
• Laboratory evaluation
LABORATORY TESTS
• Thyroid function studies
• Serum electrolytes
IMAGING STUDIES
ECG
• Regular, “sawtooth,” or “F” wave pattern, best seen in II, III, and AVF and secondary to atrial depolarization
• AV conduction block (2:1, 3:1, or varying)
TREATMENT
NONPHARMACOLOGIC THERAPY
• Valsalva maneuver or carotid sinus massage usually slows the ventricular rate (increases grade of AV block) and may make flutter waves more evident.
• Electrical cardioversion is given at low energy levels (20 to 25 J).
ACUTE GENERAL Rx
• In absence of cardioversion, IV diltiazem or digitalization may be tried to slow the ventricular rate and convert flutter to fibrillation. Esmolol, verapamil, and adenosine may also be effective.
• Atrial pacing may also terminate atrial flutter.
• Atrial flutter is frequently associated with intermittent atrial fibrillation. It may be prudent to anticoagulate patients with atrial flutter and coexisting medical disorders (e.g., diabetes mellitus, hypertension, cardiac disease) before cardioversion.
CHRONIC Rx
• Chronic atrial flutter may respond to amiodarone.
• Radiofrequency ablation to interrupt the atrial flutter is also effective for patients with chronic or recurring atrial flutter.
DISPOSITION
Over 85% of patients convert to regular sinus rhythm following cardioversion with as little as 25 to 50 J.
REFERRAL
For radiofrequency ablation in patients with chronic or recurring atrial flutter
• ECG
• Laboratory evaluation
LABORATORY TESTS
• Thyroid function studies
• Serum electrolytes
IMAGING STUDIES
ECG
• Regular, “sawtooth,” or “F” wave pattern, best seen in II, III, and AVF and secondary to atrial depolarization
• AV conduction block (2:1, 3:1, or varying)
TREATMENT
NONPHARMACOLOGIC THERAPY
• Valsalva maneuver or carotid sinus massage usually slows the ventricular rate (increases grade of AV block) and may make flutter waves more evident.
• Electrical cardioversion is given at low energy levels (20 to 25 J).
ACUTE GENERAL Rx
• In absence of cardioversion, IV diltiazem or digitalization may be tried to slow the ventricular rate and convert flutter to fibrillation. Esmolol, verapamil, and adenosine may also be effective.
• Atrial pacing may also terminate atrial flutter.
• Atrial flutter is frequently associated with intermittent atrial fibrillation. It may be prudent to anticoagulate patients with atrial flutter and coexisting medical disorders (e.g., diabetes mellitus, hypertension, cardiac disease) before cardioversion.
CHRONIC Rx
• Chronic atrial flutter may respond to amiodarone.
• Radiofrequency ablation to interrupt the atrial flutter is also effective for patients with chronic or recurring atrial flutter.
DISPOSITION
Over 85% of patients convert to regular sinus rhythm following cardioversion with as little as 25 to 50 J.
REFERRAL
For radiofrequency ablation in patients with chronic or recurring atrial flutter
Atrial flutter
BASIC INFORMATION
DEFINITION
Atrial flutter is often associated with atrial fibrillation and often requires a similar initial therapeutic approach. Atrial flutter is usually an organized atrial rhythm with an atrial rate typically between 250 and 350 b.p.m. Typical, or isthmus-dependent, atrial flutter involves a macro re-entrant right atrial circuit around the tricuspid annulus. The wavefront circulates down the lateral wall of the right atrium, through the Eustachian ridge between the tricuspid annulus and the inferior vena cava, and up the interatrial septum, giving rise to the most frequent pattern, referred to as counter-clockwise flutter. Re-entry can also occur in the opposite direction (clockwise or reverse flutter).
The ECG shows regular sawtooth-like atrial flutter waves (F waves) between QRS complexes (Fig. 15). In typical counter-clockwise atrial flutter, the F waves are negative in the inferior leads and positive in leads V1 and V2. In clockwise atrial flutter, the deflection of the F waves is the opposite. If F waves are not clearly visible, it is worth trying to reveal them by slowing AV conduction by carotid sinus massage or by the administration of AV nodal blocking drugs such as adenosine or verapamil.
Symptoms are largely related to the degree of AV block. Most often, every second flutter beat conducts, giving a ventricular rate of 150 b.p.m. Occasionally, every beat conducts, producing a heart rate of 300 b.p.m. More often, especially when patients are receiving treatment, AV conduction block reduces the heart rate to approximately 75 b.p.m.
AV Conduction.
The conduction over the AV node to the ventricles is usually 2:1. Therefore, the typical pulse during atrial flutter is usually 130-150 beats/min. Under catecholaminergic influence or in patients receiving class I antiarrhythmic therapy (e. g., flecainide), the tachycardia may show 1:1 conduction, usually with wide complexes due to rate-dependent aberration, and become life-threatening due to its rapid rate
Symptoms are largely related to the degree of AV block. Most often, every second flutter beat conducts, giving a ventricular rate of 150 b.p.m. Occasionally, every beat conducts, producing a heart rate of 300 b.p.m. More often, especially when patients are receiving treatment, AV conduction block reduces the heart rate to approximately 75 b.p.m.
AV Conduction.
The conduction over the AV node to the ventricles is usually 2:1. Therefore, the typical pulse during atrial flutter is usually 130-150 beats/min. Under catecholaminergic influence or in patients receiving class I antiarrhythmic therapy (e. g., flecainide), the tachycardia may show 1:1 conduction, usually with wide complexes due to rate-dependent aberration, and become life-threatening due to its rapid rate
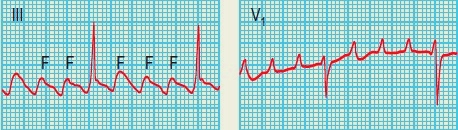
Fig. 15 Atrial flutter. Some flutter waves are marked with an F. In this case the flutter frequency is 240/min. Every fourth flutter wave is transmitted to the ventricles and the ventricular rate is therefore 60/min.
Conversely, the AV conduction may slow down (e. g., 3:1 or 4:1) with carotid massage or by application of various drugs resulting in the unmasking of the flutter waves (Fig. 15.1). The ventricular rate during atrial flutter has a certain regularity, differentiating it from atrial fibrillation, which has a totally irregular rhythm. Atrial flutter is responsive to curative therapy with radiofrequency catheter ablation in which the macroreentry is interrupted at a narrow electrical isthmus.
Conversely, the AV conduction may slow down (e. g., 3:1 or 4:1) with carotid massage or by application of various drugs resulting in the unmasking of the flutter waves (Fig. 15.1). The ventricular rate during atrial flutter has a certain regularity, differentiating it from atrial fibrillation, which has a totally irregular rhythm. Atrial flutter is responsive to curative therapy with radiofrequency catheter ablation in which the macroreentry is interrupted at a narrow electrical isthmus.

EPIDEMIOLOGY & DEMOGRAPHICS
Atrial flutter is common during the first week after open heart surgery.
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Fast pulse rate (approximately 150 bpm)
• Symptoms of cardiac failure, light-headedness, and angina pectoris
ETIOLOGY
• Atherosclerotic heart disease
• MI
• Thyrotoxicosis
• Pulmonary embolism
• Mitral valve disease
• Cardiac surgery
• COPD
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
• Atrial fibrillation
• Paroxysmal atrial tachycardia
Atrial flutter is common during the first week after open heart surgery.
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Fast pulse rate (approximately 150 bpm)
• Symptoms of cardiac failure, light-headedness, and angina pectoris
ETIOLOGY
• Atherosclerotic heart disease
• MI
• Thyrotoxicosis
• Pulmonary embolism
• Mitral valve disease
• Cardiac surgery
• COPD
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
• Atrial fibrillation
• Paroxysmal atrial tachycardia
Fig. 15.1 Atrial flutter with 2:1 conduction converting into 1:1 conduction with aberration. The initial tachycardia is regular at a rate of 150 beats/min and has a narrow complex. The second tachycardia is exactly twice as fast as the initial tachycardia, which is unlikely to occur by chance. If the initial tachycardia were not documented, it would be difficult to differentiate atrial flutter from ventricular tachycardia in this patient.
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!