Induced Immunity
Immunity occurs naturally through infection or is brought about artificially (induced) by medical intervention. The two types of induced immunity are active and passive. In active immunity, the individual alone produces antibodies against an antigen; in passive immunity, the individual is given prepared antibodies via an injection.
Active Immunity
Active immunity sometimes develops naturally after a person is infected with a pathogen. However, active immunity is often induced when a person is well so that future infection will not take place. To prevent infections, people are immunized artificially against them. The United States is committed to immunizing all children against the common types of childhood disease.
Immunization involves the use of vaccines, substances that contain an antigen to which the immune system responds. Traditionally, vaccines are the pathogens themselves, or their products, that have been treated so they are no longer virulent (able to cause disease). Today, it is possible to genetically engineer bacteria to mass-produce a protein from pathogens, and this protein can be used as a vaccine. This method has now produced a vaccine against hepatitis B, a viral- induced disease, and is being used to prepare a vaccine against malaria, a protozoan-induced disease. After a vaccine is given, it is possible to follow an immune response by determining the amount of antibody present in a sample of plasma-this is called the antibody titer. After the first exposure to a vaccine, a primary response occurs. For a period of several days, no antibodies are present; then the titer rises slowly, levels off, and gradually declines as the antibodies bind to the antigen or simply break down (Fig. 13.9). After a second exposure to the vaccine, a secondary response is expected. The titer rises rapidly to a level much greater than before; then it slowly declines. The second exposure is called a “booster” because it boosts the antibody titer to a high level. The high antibody titer now is expected to help prevent disease symptoms even if the individual is exposed to the disease-causing antigen.
Active immunity is dependent upon the presence of memory B cells and memory T cells that are capable of responding to lower doses of antigen. Active immunity is usually long-lasting, although a booster may be required every so many years.
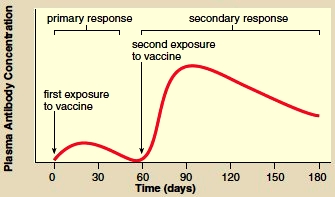
Figure 13.9 During immunization, the primary response, after the first exposure to a vaccine, is minimal, but the secondary response, which may occur after the second exposure, shows a dramatic rise in the amount of antibody present in plasma.
Passive Immunity
Passive immunity occurs when an individual is given prepared antibodies (immunoglobulins) to combat a disease. Since these antibodies are not produced by the individual’s plasma cells, passive immunity is temporary. For example, newborn infants are passively immune to some diseases because antibodies have crossed the placenta from the mother’s blood. These antibodies soon disappear, however, so that within a few months, infants become more susceptible to infections. Breast-feeding prolongs the natural passive immunity an infant receives from the mother because antibodies are present in the mother’s milk (Fig. 13.10). Even though passive immunity does not last, it is sometimes used to prevent illness in a patient who has been unexpectedly exposed to an infectious disease. Usually, the patient receives a gamma globulin injection (serum that contains antibodies), perhaps taken from individuals who have recovered from the illness. In the past, horses were immunized, and serum was taken from them to provide the needed antibodies against such diseases as diphtheria, botulism, and tetanus.
Unfortunately, a patient who received these antibodies became ill about 50% of the time, because the serum contained proteins that the individual’s immune system recognized as foreign. This was called serum sickness. But problems can also occur with products made in other ways. An immunoglobulin intravenous product called Gammagard was withdrawn from the market because of its possible implication in the transmission of hepatitis.
Every plasma cell derived from the same B cell secretes antibodies against a specific antigen. These are monoclonal antibodies because all of them are the same type and because they are produced by plasma cells derived from the same B cell. One method of producing monoclonal antibodies in vitro (outside the body in glassware) is depicted in Figure 13.11. B lymphocytes are removed from an animal (today, usually mice are used) and are exposed to a particular antigen.
Monoclonal Antibodies
Every plasma cell derived from the same B cell secretes antibodies against a specific antigen. These are monoclonal antibodies because all of them are the same type and because they are produced by plasma cells derived from the same B cell. One method of producing monoclonal antibodies in vitro (outside the body in glassware) is depicted in Figure 13.11. B lymphocytes are removed from an animal (today, usually mice are used) and are exposed to a particular antigen.

Figure 13.10 Passive immunity. Breast-feeding is believed to prolong the passive immunity an infant receives from the mother because antibodies are present in the mother’s milk.
The resulting plasma cells are fused with myeloma cells (malignant plasma cells that live and divide indefinitely). The fused cells are called hybridomas-hybrid- because they result from the fusion of two different cells, and -oma because one of the cells is a cancer cell.
At present, monoclonal antibodies are being used for quick and certain diagnosis of various conditions. For example, a particular hormone is present in the urine of a pregnant woman. A monoclonal antibody can be used to detect this hormone; if it is present, the woman knows she is pregnant. Monoclonal antibodies are also used to identify infections. And because they can distinguish between cancerous and normal tissue cells, they are used to carry radioactive isotopes or toxic drugs to tumors, which can then be selectively destroyed.
At present, monoclonal antibodies are being used for quick and certain diagnosis of various conditions. For example, a particular hormone is present in the urine of a pregnant woman. A monoclonal antibody can be used to detect this hormone; if it is present, the woman knows she is pregnant. Monoclonal antibodies are also used to identify infections. And because they can distinguish between cancerous and normal tissue cells, they are used to carry radioactive isotopes or toxic drugs to tumors, which can then be selectively destroyed.
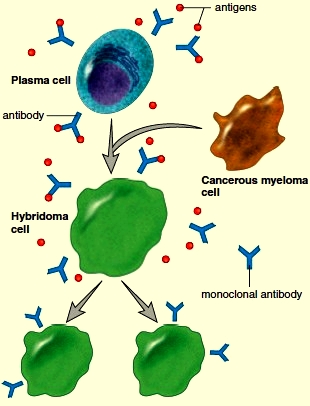
Figure 13.11 Production of monoclonal antibodies. Plasma cells of the same type (derived from immunized mice) are fused with myeloma (cancerous) cells, producing hybridoma cells that are “immortal.” Hybridoma cells divide and continue to produce the same type of antibody, called monoclonal antibodies.
Tissue Rejection
Certain organs, such as skin, the heart, and the kidneys, could be transplanted easily from one person to another if the body did not attempt to reject them. Rejection of transplanted tissue results because the recipient’s immune system recognizes that the transplanted tissue is not “self.” Cytotoxic T cells respond by causing disintegration of the transplanted tissue. Organ rejection can be controlled by carefully selecting the organ to be transplanted and administering immunosuppressive drugs. It is best if the transplanted organ has the same type of HLA antigens as those of the recipient, because T cells recognize foreign HLA antigens. Two well-known immunosuppressive drugs, cyclosporine and tacrolimus, both act by inhibiting the response of T cells to cytokines. Researchers hope that tissue engineering, including the production of organs that lack antigens or that can be protected in some way from the immune system, will one day do away with the problem of rejection.
Diseases of the Immune System
When a person has an autoimmune disease, cytotoxic T cells or antibodies mistakenly attack the body’s own cells as if they bear foreign antigens. Exactly what causes autoimmune diseases is not known. However, sometimes they occur after an individual has recovered from an infection. In the autoimmune disease myasthenia gravis, neuromuscular junctions do not work properly, and muscular weakness results. In multiple sclerosis (MS), the myelin sheath of nerve fibers breaks down, and this causes various neuromuscular disorders. A person with systemic lupus erythematosus (SLE) has various symptoms prior to death due to kidney damage. In rheumatoid arthritis, the joints are affected. Researchers suggest that heart damage following rheumatic fever and type I diabetes are also autoimmune illnesses. As yet, there are no cures for autoimmune diseases, but they can be controlled with drugs. When a person has an immune deficiency, the immune system is unable to protect the body against disease. AIDS is an example of an acquired immune deficiency. As a result of a weakened immune system, AIDS patients show a greater susceptibility to a variety of diseases, and also have a higher risk of cancer. Immune deficiency may also be congenital (that is, inherited). Infrequently, a child may be born with an impaired B- or T-cell system caused by a defect in lymphocyte development. In severe combined immunodeficiency disease (SCID), both antibody- and cell-mediated immunity are lacking or inadequate. Without treatment, even common infections can be fatal. Gene therapy has been successful in SCID patients.
Immunity Side Effects
The immune system usually protects us from disease because it can distinguish self from nonself. Sometimes, however, it responds in a manner that harms the body, as when individuals develop allergies, suffer tissue rejection, or have an autoimmune disease.
Allergies
Allergies are hypersensitivities to substances such as pollen or animal hair that ordinarily would do no harm to the body. The response to these antigens, called allergens, usually includes some degree of tissue damage. There are four types of allergic responses, but we will consider only two of them: immediate allergic response and delayed allergic response.
Immediate Allergic Response
An immediate allergic response can occur within seconds of contact with the antigen. The response is caused by antibodies known as IgE (see Table 13.1). IgE antibodies are attached to the plasma membrane of mast cells in the tissues and also to basophils in the blood. When an allergen attaches to the IgE antibodies on these cells, mast cells release histamine and other substances that bring about the allergic symptoms. When pollen is an allergen, histamine stimulates the mucosal membranes of the nose and eyes to release fluid, causing the runny nose and watery eyes typical of hay fever. If a person has asthma, the airways leading to the lungs constrict, resulting in difficult breathing accompanied by wheezing. When food contains an allergen, nausea, vomiting, and diarrhea result.
Anaphylactic shock is an immediate allergic response that occurs because the allergen has entered the bloodstream. Bee stings and penicillin shots are known to cause this reaction because both inject the allergen into the blood. Anaphylactic shock is characterized by a sudden and life-threatening drop in blood pressure due to increased permeability of the capillaries by histamine. Taking epinephrine can delay this reaction until medical help is available. Allergy shots sometimes prevent the onset of immediate allergic responses. It has been suggested that injections of the allergen may cause the body to build up high quantities of IgG antibodies, and these combine with allergens received from the environment before they have a chance to reach the IgE antibodies located in the membrane of mast cells and basophils. Delayed Allergic Response A delayed allergic response is initiated by memory T cells at the site of allergen contact in the body. The allergic response is regulated by the cytokines secreted by both T cells and macrophages. A classic example of a delayed allergic response is the skin test for tuberculosis (TB). When the test result is positive, the tissue where the antigen was injected becomes red and hardened. This shows that there was prior exposure to tubercle bacilli, the cause of TB. Contact dermatitis, which occurs when a person is allergic to poison ivy, jewelry, cosmetics, and many other substances that touch the skin, is also an example of a delayed allergic response.
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!