Arthritis, infectious (bacterial)
DEFINITION
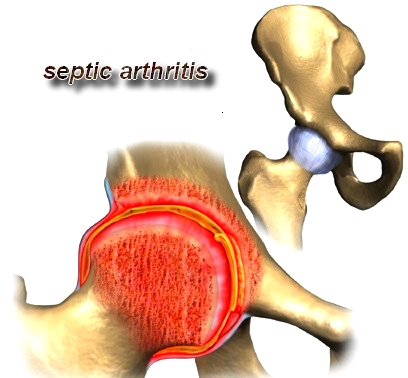
Bacterial arthritis is a highly destructive form of joint disease most often caused by hematogenous spread of organisms from a distant site of infection. Direct penetration of the joint as a result of trauma or surgery and spread from adjacent osteomyelitis may also cause bacterial arthritis. Any joint in the body may be affected. Gonococcal arthritis causes a distinct clinical syndrome and is often considered separately.
SYNONYMS
Septic arthritis
Pyogenic arthritis
CAUSES
In most cases of septic arthritis, bacteria spread from a primary site of infection, usually in adjacent bone or soft tissue, through the bloodstream to the joint. Common infecting organisms include:
* four strains of gram-positive cocci - Staphylococcus aureus, Streptococcus pyogenes, Streptococcus pneumoniae, and Streptococcus viridans
* two strains of gram-negative cocci - Neisseria gonorrhoeae and Haemophilus influenzae
* various gram-negative bacilli, including Escherichia coli, Salmonella, and Pseudomonas.
Septic arthritis
Pyogenic arthritis
CAUSES
In most cases of septic arthritis, bacteria spread from a primary site of infection, usually in adjacent bone or soft tissue, through the bloodstream to the joint. Common infecting organisms include:
* four strains of gram-positive cocci - Staphylococcus aureus, Streptococcus pyogenes, Streptococcus pneumoniae, and Streptococcus viridans
* two strains of gram-negative cocci - Neisseria gonorrhoeae and Haemophilus influenzae
* various gram-negative bacilli, including Escherichia coli, Salmonella, and Pseudomonas.

Rarely, fungi or mycobacteria cause the infection. Anaerobic organisms such as gram-positive cocci may infect children over age 2 and adults. H. influenzae most often infects children under age 2.
Various factors can predispose a person to septic arthritis. Any concurrent bacterial infection (of the genitourinary or upper respiratory tract, for example) or serious chronic illness (such as cancer, renal failure, rheumatoid arthritis, septic lupus erythematosus, diabetes, or cirrhosis) heightens susceptibility. Consequently, alcoholics and the elderly run an increased risk of developing septic arthritis.
Susceptibility also increases among patients with immune system depression or a history of immunosuppressive therapy. I.V. drug abuse can also lead to septic arthritis. Other predisposing factors include recent articular trauma, joint surgery, intra-articular injections, and local joint abnormalities.
EPIDEMIOLOGY & DEMOGRAPHICS
INCIDENCE (IN U.S.): Unknown
PREVALENCE (IN U.S.): Unknown
PREDOMINANT SEX: Gonococcal arthritis in males
PREDOMINANT AGE: Gonococcal arthritis in sexually active adults
PEAK INCIDENCE:
• Gonococcal arthritis: young adults
• Other bacterial causes: all ages
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Hallmark: acute onset of a swollen, painful joint
• Limited range of motion of the joint
• Effusion, with varying degrees of erythema and increased warmth around the joint
• Single joint affected in 80% to 90% of cases of nongonococcal arthritis
• Gonococcal dermatitis-arthritis syndrome
1. Typical pattern is a migratory polyarthritis or tenosynovitis
2. Small pustules on the trunk or extremities
• Febrile patient at presentation
• Most commonly affected joints in adult: knee and hip, but any joint may be involved; in children: hip
ETIOLOGY
• Bacteria spread from another locus of infection
1. Highly vascular synovium is invaded by hematogenously spread bacteria.
2. WBC enzymes cause necrosis of synovium, cartilage, and bone.
3. Extensive joint destruction is rapid if infection is not treated with appropriate IV antibiotics and drainage of necrotic material.
• Predisposing factors: rheumatoid arthritis, prosthetic joints, advanced age, immunodeficiency
• The most common nongonococcal organisms are Staphylococcus aureus, b-hemolytic streptococci, and gram-negative bacilli.
DIAGNOSIS
• Gout
• Pseudogout
• Trauma
• Hemarthrosis
• Rheumatic fever
• Adult or juvenile rheumatoid arthritis
• Spondyloarthropathies such as Reiter’s syndrome
• Osteomyelitis
• Viral arthritides
• Septic bursitis
Various factors can predispose a person to septic arthritis. Any concurrent bacterial infection (of the genitourinary or upper respiratory tract, for example) or serious chronic illness (such as cancer, renal failure, rheumatoid arthritis, septic lupus erythematosus, diabetes, or cirrhosis) heightens susceptibility. Consequently, alcoholics and the elderly run an increased risk of developing septic arthritis.
Susceptibility also increases among patients with immune system depression or a history of immunosuppressive therapy. I.V. drug abuse can also lead to septic arthritis. Other predisposing factors include recent articular trauma, joint surgery, intra-articular injections, and local joint abnormalities.
EPIDEMIOLOGY & DEMOGRAPHICS
INCIDENCE (IN U.S.): Unknown
PREVALENCE (IN U.S.): Unknown
PREDOMINANT SEX: Gonococcal arthritis in males
PREDOMINANT AGE: Gonococcal arthritis in sexually active adults
PEAK INCIDENCE:
• Gonococcal arthritis: young adults
• Other bacterial causes: all ages
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Hallmark: acute onset of a swollen, painful joint
• Limited range of motion of the joint
• Effusion, with varying degrees of erythema and increased warmth around the joint
• Single joint affected in 80% to 90% of cases of nongonococcal arthritis
• Gonococcal dermatitis-arthritis syndrome
1. Typical pattern is a migratory polyarthritis or tenosynovitis
2. Small pustules on the trunk or extremities
• Febrile patient at presentation
• Most commonly affected joints in adult: knee and hip, but any joint may be involved; in children: hip
ETIOLOGY
• Bacteria spread from another locus of infection
1. Highly vascular synovium is invaded by hematogenously spread bacteria.
2. WBC enzymes cause necrosis of synovium, cartilage, and bone.
3. Extensive joint destruction is rapid if infection is not treated with appropriate IV antibiotics and drainage of necrotic material.
• Predisposing factors: rheumatoid arthritis, prosthetic joints, advanced age, immunodeficiency
• The most common nongonococcal organisms are Staphylococcus aureus, b-hemolytic streptococci, and gram-negative bacilli.
DIAGNOSIS
• Gout
• Pseudogout
• Trauma
• Hemarthrosis
• Rheumatic fever
• Adult or juvenile rheumatoid arthritis
• Spondyloarthropathies such as Reiter’s syndrome
• Osteomyelitis
• Viral arthritides
• Septic bursitis

WORKUP
• Joint aspiration, Gram stain, and culture of the synovial fluid
• Immediate arthrocentesis before other studies are undertaken or antibiotics instituted
LABORATORY TESTS
• Joint fluid analysis
1. Synovial fluid leukocyte count is usually elevated >50,000 cells/mm3 with a differential count of 80% or more polymorphonuclear cells.
2. Counts are highly variable, with similar findings in gout, pseudogout, or rheumatoid arthritis.
3. The differential diagnosis of sy-novial fluid abnormalities is described in Table 2-192.
• Blood cultures
• Culture of possible extraarticular sources of infection
• Elevated peripheral WBC count and ESR (nonspecific)
IMAGING STUDIES
• X-ray examination of the affected joint to rule out osteomyelitis
• CT scan for early diagnosis of infections of the spine, hips, and sternoclavicular and sacroiliac joints
• Technetium and gallium scintigraphic scans (positive, but do not permit differentiation of infection from inflammation)
• Indium-labeled WBC scans (less sensitive, but more specific)
TREATMENT
Treatment for septic arthritis requires monitoring of progress through frequent analysis of joint fluid cultures, synovial fluid leukocyte counts, and glucose determinations. Bioassays or bactericidal assays of synovial fluid and bioassays of blood may confirm clearing of the infection. Codeine or propoxyphene can be given for pain, if needed. (Aspirin misleadingly reduces swelling and may mask fever, hindering accurate monitoring of progress.) The joint may be immobilized with a splint or put into traction until the patient can tolerate movement. As the infection resolves, exercise is added to the treatment regimen to restore strength and mobility.
Needle aspiration (arthrocentesis) to remove grossly purulent joint fluid may be repeated daily until the fluid appears normal. If cultures remain positive or the WBC count remains elevated, the patient may need arthroscopic surgical drainage to remove resistant infection. (Septic arthritis of the hip requires open surgical drainage.)
Reconstructive surgery is warranted only for severe joint damage and only after all signs of active infection disappear. This usually takes several months. The patient is likely to need arthroplasty or joint fusion. Prosthetic replacement is controversial because it may exacerbate the infection; it has been used successfully when the femoral head or acetabulum has sustained damage.
NONPHARMACOLOGIC THERAPY
• Affected joints aspirated daily to remove necrotic material and to follow serial WBC counts and cultures
• If no resolution with IV antibiotics and closed drainage: open debridement and lavage, particularly in nongonococcal infections
• Prevention of contractures:
1. After acute stage of inflammation, range-of-motion exercises of the affected joint
2. Physical therapy helpful
ACUTE GENERAL Rx
• IV antibiotics immediately after joint aspiration and Gram stain of the synovial fluid
• For infections caused by grampositive cocci: penicillinase-resistant penicillin, such as nafcillin (2 g IV q4h), unless there is clinical suspicion of methicillin resistant
Staphylococcus aureus, in which case vancomycin (1 g IV q12h)
• Infections caused by gram-negative bacilli: treated with a thirdgeneration cephalosporin or an anti-pseudomonal penicillin plus an aminoglycoside, pending C&S results
• For suspected gonococcal infection, including young adults when the synovial fluid Gram stain is nondiagnostic: ceftriaxone 1 g IV q24h
DISPOSITION
• With prompt treatment, complete resolution is expected.
• Delay in treatment may result in permanent destruction of cartilage and loss of function of the affected joint.
• Joint aspiration, Gram stain, and culture of the synovial fluid
• Immediate arthrocentesis before other studies are undertaken or antibiotics instituted
LABORATORY TESTS
• Joint fluid analysis
1. Synovial fluid leukocyte count is usually elevated >50,000 cells/mm3 with a differential count of 80% or more polymorphonuclear cells.
2. Counts are highly variable, with similar findings in gout, pseudogout, or rheumatoid arthritis.
3. The differential diagnosis of sy-novial fluid abnormalities is described in Table 2-192.
• Blood cultures
• Culture of possible extraarticular sources of infection
• Elevated peripheral WBC count and ESR (nonspecific)
IMAGING STUDIES
• X-ray examination of the affected joint to rule out osteomyelitis
• CT scan for early diagnosis of infections of the spine, hips, and sternoclavicular and sacroiliac joints
• Technetium and gallium scintigraphic scans (positive, but do not permit differentiation of infection from inflammation)
• Indium-labeled WBC scans (less sensitive, but more specific)
TREATMENT
Treatment for septic arthritis requires monitoring of progress through frequent analysis of joint fluid cultures, synovial fluid leukocyte counts, and glucose determinations. Bioassays or bactericidal assays of synovial fluid and bioassays of blood may confirm clearing of the infection. Codeine or propoxyphene can be given for pain, if needed. (Aspirin misleadingly reduces swelling and may mask fever, hindering accurate monitoring of progress.) The joint may be immobilized with a splint or put into traction until the patient can tolerate movement. As the infection resolves, exercise is added to the treatment regimen to restore strength and mobility.
Needle aspiration (arthrocentesis) to remove grossly purulent joint fluid may be repeated daily until the fluid appears normal. If cultures remain positive or the WBC count remains elevated, the patient may need arthroscopic surgical drainage to remove resistant infection. (Septic arthritis of the hip requires open surgical drainage.)
Reconstructive surgery is warranted only for severe joint damage and only after all signs of active infection disappear. This usually takes several months. The patient is likely to need arthroplasty or joint fusion. Prosthetic replacement is controversial because it may exacerbate the infection; it has been used successfully when the femoral head or acetabulum has sustained damage.
NONPHARMACOLOGIC THERAPY
• Affected joints aspirated daily to remove necrotic material and to follow serial WBC counts and cultures
• If no resolution with IV antibiotics and closed drainage: open debridement and lavage, particularly in nongonococcal infections
• Prevention of contractures:
1. After acute stage of inflammation, range-of-motion exercises of the affected joint
2. Physical therapy helpful
ACUTE GENERAL Rx
• IV antibiotics immediately after joint aspiration and Gram stain of the synovial fluid
• For infections caused by grampositive cocci: penicillinase-resistant penicillin, such as nafcillin (2 g IV q4h), unless there is clinical suspicion of methicillin resistant
Staphylococcus aureus, in which case vancomycin (1 g IV q12h)
• Infections caused by gram-negative bacilli: treated with a thirdgeneration cephalosporin or an anti-pseudomonal penicillin plus an aminoglycoside, pending C&S results
• For suspected gonococcal infection, including young adults when the synovial fluid Gram stain is nondiagnostic: ceftriaxone 1 g IV q24h
DISPOSITION
• With prompt treatment, complete resolution is expected.
• Delay in treatment may result in permanent destruction of cartilage and loss of function of the affected joint.
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!