Table 18.1 Nomenclature of bone tumors
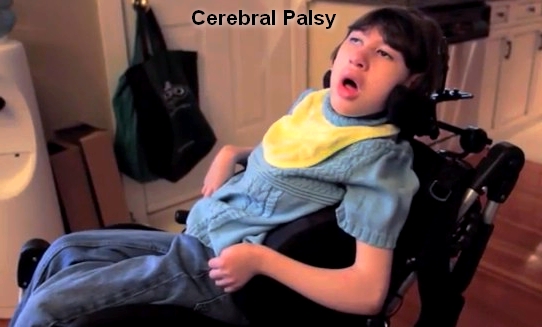
Cerebral palsy
BASIC INFORMATION
DEFINITION
Cerebral palsy encompasses disorders apparent at birth or in childhood due to intra-uterine or neonatal brain damage; deficits are non-progressive. Learning problems, mild to severe, are frequent, though not exclusive - physical disability is independent of cognitive impairment. The precise cause of damage in an individual child may be difficult to determine. The following are largely responsible:
■ hypoxia in utero and/or during parturition
■ neonatal cerebral haemorrhage and/or infarction
■ trauma, neonatal or during parturition
■ prolonged seizures - status epilepticus
■ hypoglycaemia
■ kernicterus with athetoid movement disorder - now rare with maternal Rh immunization.
SYNONYMS
Little’s disease
Congenital static encephalopathy
Congenital spastic paralysis
Clinical features
Failure to achieve normal milestones is usually the earliest feature. Specific motor syndromes become apparent later in childhood or, rarely, in adult life.
■ Spastic diplegia is spasticity, predominantly of lower limbs, with scissoring of gait.
■ Athetoid cerebral palsy.
■ Infantile hemiparesis. Hemiparesis may be noted at birth or later. One hemisphere is hypotrophic and the contralateral, hemiparetic limbs small (hemiatrophy).
■ Congenital ataxia is incoordination and hypotonia of limbs and trunk.
EPIDEMIOLOGY & DEMOGRAPHICS
INCIDENCE (IN U.S.): 1.5 to 2.5 cases / 1000 live births
PREVALENCE (IN U.S.): Close to incidence (0 nonprogressive disease)
PREDOMINANT SEX: Male = female
PREDOMINANT AGE: 3 to 5 years
PEAK INCIDENCE: At birth
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Mental retardation (35%)
• Seizures (35%)
• Hemiplegia
• Diplegia
• Extrapyramidal findings
• Delay in motor milestones
• Hypotonia
ETIOLOGY
Multifactorial: low birth weight, congenital malformations, thyroid or estrogen therapy during pregnancy, low Apgar scores, difficult delivery, prematurity, hyperbilirubinemia
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
Spinal cord abnormalities
Failure to achieve normal milestones is usually the earliest feature. Specific motor syndromes become apparent later in childhood or, rarely, in adult life.
■ Spastic diplegia is spasticity, predominantly of lower limbs, with scissoring of gait.
■ Athetoid cerebral palsy.
■ Infantile hemiparesis. Hemiparesis may be noted at birth or later. One hemisphere is hypotrophic and the contralateral, hemiparetic limbs small (hemiatrophy).
■ Congenital ataxia is incoordination and hypotonia of limbs and trunk.
EPIDEMIOLOGY & DEMOGRAPHICS
INCIDENCE (IN U.S.): 1.5 to 2.5 cases / 1000 live births
PREVALENCE (IN U.S.): Close to incidence (0 nonprogressive disease)
PREDOMINANT SEX: Male = female
PREDOMINANT AGE: 3 to 5 years
PEAK INCIDENCE: At birth
PHYSICAL FINDINGS & CLINICAL PRESENTATION
• Mental retardation (35%)
• Seizures (35%)
• Hemiplegia
• Diplegia
• Extrapyramidal findings
• Delay in motor milestones
• Hypotonia
ETIOLOGY
Multifactorial: low birth weight, congenital malformations, thyroid or estrogen therapy during pregnancy, low Apgar scores, difficult delivery, prematurity, hyperbilirubinemia
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
Spinal cord abnormalities
WORKUP
Follow motor milestones and primitive reflexes
LABORATORY TESTS
• Thyroid function
• Urine amino acid screen
• Chromosomal analysis
IMAGING STUDIES
CT scan, MRI, and ultrasonography may show periventricular leukomalacia and/or periventricular hemorrhage.
TREATMENT
NONPHARMACOLOGIC THERAPY
• Physical therapy
• Special education
ACUTE GENERAL Rx
Not applicable unless seizures are present.
CHRONIC Rx
• Physical therapy
• Special schooling
• Treatment of seizures, if present
• Intrathecal baclofen
• Botulinum toxin
DISPOSITION
Have child remain at home if at all possible.
Follow motor milestones and primitive reflexes
LABORATORY TESTS
• Thyroid function
• Urine amino acid screen
• Chromosomal analysis
IMAGING STUDIES
CT scan, MRI, and ultrasonography may show periventricular leukomalacia and/or periventricular hemorrhage.
TREATMENT
NONPHARMACOLOGIC THERAPY
• Physical therapy
• Special education
ACUTE GENERAL Rx
Not applicable unless seizures are present.
CHRONIC Rx
• Physical therapy
• Special schooling
• Treatment of seizures, if present
• Intrathecal baclofen
• Botulinum toxin
DISPOSITION
Have child remain at home if at all possible.
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!