Epidermis
The epidermis is the superficial protective layer of the skin. Derived from ectoderm, the epidermis is composed of stratified squamous epithelium that varies in thickness from 0.007 to 0.12 mm. All but the deepest layers are composed of dead cells. Either four or five layers may be present, depending on where the epidermis is located (figs. 2.1 and 2.2). The epidermis of the palms and soles has five layers because these areas are exposed to the most friction. In all other areas of the body, the epidermis has only four layers. The names and characteristics of the epidermal layers are as follows.
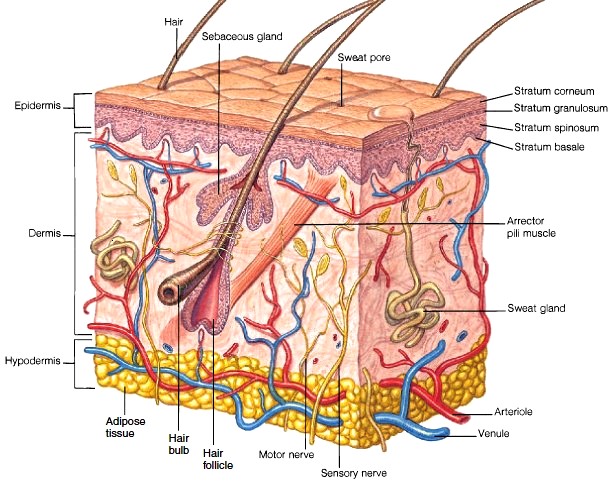
FIGURE 2.1 A diagram of the skin.

FIGURE 2.2 A light micrograph of the epidermis
1. Stratum basale (basal layer).The stratum basale consists of a single layer of cells in contact with the dermis. Four types of cells compose the stratum basale: keratinocytes, melanocytes, tactile cells (Merkel cells), and nonpigmented granular dendrocytes (Langerhans cells). With the exception of tactile cells, these cells are constantly dividing mitotically and moving outward to renew the epidermis. It usually takes between 6 to 8 weeks for the cells to move from the stratum basale to the surface of the skin. Keratinocytes are specialized cells that produce the protein keratin, which toughens and waterproofs the skin. As keratinocytes are pushed away from the vascular nutrient and oxygen supply of the dermis, their nuclei degenerate, their cellular content becomes dominated by keratin, and the process of keratinization is completed. By the time keratinocytes reach the surface of the skin, they resemble flat dead scales. They are completely filled with keratin enclosed in loose cell membranes. Melanocytes are specialized epithelial cells that synthesize the pigment melanin which provides a protective barrier to the ultraviolet radiation in sunlight. Tactile cells are sparse compared to keratinocytes and melanocytes. These sensory receptor cells aid in tactile (touch) reception. Nonpigmented granular dendrocytes are scattered throughout the stratum basale. They are protective macrophagic cells that ingest bacteria and other foreign debris.
2. Stratum spinosum (spiny layer).The stratum spinosum contains several layers of cells. The spiny appearance of this layer is due to the spinelike extensions that arise from the keratinocytes when the tissue is fixed for microscopic examination. Because there is limited mitosis in the stratum spinosum, this layer and the stratum basale are collectively referred to as the stratum germinativum.
3. Stratum granulosum (granular layer).The stratum granulosum consists of only three or four flattened layers of cells. These cells contain granules that are filled with keratohyalin, a chemical precursor to keratin.
4. Stratum lucidum (clear layer).The nuclei, organelles, and cell membranes are no longer visible in the cells of the stratum lucidum, and so histologically this layer appears clear. It exists only in the lips and in the thickened skin of the soles and palms.
5. Stratum corneum (hornlike layer).The stratum corneum is composed of 25 to 30 layers of flattened, scalelike cells. Thousands of these dead cells shed from the skin surface each day, only to be replaced by new ones from deeper layers. This surface layer is cornified; it is the layer that actually protects the skin (fig. 2.3). Cornification, brought on by keratinization, is the drying and flattening of the stratum corneum and is an important protective adaptation of the skin. Friction at the surface of the skin stimulates additional mitotic activity in the stratum basale and stratum spinosum, which may result in the formation of a callus for additional protection. The specific characteristics of each epidermal layer are described in pic. 1.
2. Stratum spinosum (spiny layer).The stratum spinosum contains several layers of cells. The spiny appearance of this layer is due to the spinelike extensions that arise from the keratinocytes when the tissue is fixed for microscopic examination. Because there is limited mitosis in the stratum spinosum, this layer and the stratum basale are collectively referred to as the stratum germinativum.
3. Stratum granulosum (granular layer).The stratum granulosum consists of only three or four flattened layers of cells. These cells contain granules that are filled with keratohyalin, a chemical precursor to keratin.
4. Stratum lucidum (clear layer).The nuclei, organelles, and cell membranes are no longer visible in the cells of the stratum lucidum, and so histologically this layer appears clear. It exists only in the lips and in the thickened skin of the soles and palms.
5. Stratum corneum (hornlike layer).The stratum corneum is composed of 25 to 30 layers of flattened, scalelike cells. Thousands of these dead cells shed from the skin surface each day, only to be replaced by new ones from deeper layers. This surface layer is cornified; it is the layer that actually protects the skin (fig. 2.3). Cornification, brought on by keratinization, is the drying and flattening of the stratum corneum and is an important protective adaptation of the skin. Friction at the surface of the skin stimulates additional mitotic activity in the stratum basale and stratum spinosum, which may result in the formation of a callus for additional protection. The specific characteristics of each epidermal layer are described in pic. 1.

FIGURE 2.3 A scanning electron micrograph of the surface of the skin showing the opening of a sweat gland.

Pic. 1. Layers of the Epidermis
Coloration of the Skin
Normal skin color is the expression of a combination of three pigments: melanin, carotene, and hemoglobin. Melanin is a brownblack pigment produced in the melanocytes of the stratum basale (fig. 2.4). All individuals of similar size have approximately the same number of melanocytes, but the amount of melanin produced and the distribution of the melanin determine racial variations in skin color, such as black, brown, yellow, and white. Melanin protects the basal layer against the damaging effect of the ultraviolet (UV) rays of the sun. A gradual exposure to the sunlight promotes the increased production of melanin within the melanocytes, and hence tanning of the skin. The skin of a person with albinism has the normal number of melanocytes in the epidermis but lacks the enzyme tyrosinase that converts the amino acid tyrosine to melanin. Albinism is a hereditary condition. Other genetic expressions of melanocytes are more common than albinism. Freckles, for example, are caused by aggregated patches of melanin. A lack of melanocytes in localized areas of the skin causes distinct white spots in the condition called vitiligo. After the age of 50, brown plaquelike growths, called seborrheic hyperkeratoses, may appear on the skin, particularly on exposed portions. Commonly called “liver spots,” these pigmented patches are benign growths of pigment-producing melanocytes. Usually no treatment is required, unless for cosmetic purposes.
Carotene is a yellowish pigment found in certain plant products, such as carrots, that tends to accumulate in cells of the stratum corneum and fatty parts of the dermis. It was once thought to account for the yellow-tan skin of people of Asian descent, but this coloration is now known to be caused by variations in melanin.
Hemoglobin is not a pigment of the skin; rather, it is the oxygen-binding pigment found in red blood cells. Oxygenated blood flowing through the dermis gives the skin its pinkish tones.

FIGURE 2.4 Melanocytes throughout the stratum basale (see arrow) produce melanin.

Surface Patterns
The exposed surface of the skin has recognizable patterns that are either present at birth or develop later. Fingerprints (friction ridges) are congenital patterns that are present on the finger and toe pads, as well as on the palms and soles. The designs formed by these lines have basic similarities but are not identical in any two individuals (fig. 2.5). They are formed by the pull of elastic fibers within the dermis and are well established prenatally. The ridges of fingerprints function to prevent slippage when grasping objects. Because they are precise and easy to reproduce, fingerprints are customarily used for identifying individuals. Acquired lines include the deep flexion creases on the palms and the shallow flexion lines that can be seen on the knuckles and on the surface of other joints. Furrows on the forehead and face are acquired from continual contraction of facial muscles, such as from smiling or squinting in bright light or against the wind. Facial lines become more strongly delineated as a person ages.
The exposed surface of the skin has recognizable patterns that are either present at birth or develop later. Fingerprints (friction ridges) are congenital patterns that are present on the finger and toe pads, as well as on the palms and soles. The designs formed by these lines have basic similarities but are not identical in any two individuals (fig. 2.5). They are formed by the pull of elastic fibers within the dermis and are well established prenatally. The ridges of fingerprints function to prevent slippage when grasping objects. Because they are precise and easy to reproduce, fingerprints are customarily used for identifying individuals. Acquired lines include the deep flexion creases on the palms and the shallow flexion lines that can be seen on the knuckles and on the surface of other joints. Furrows on the forehead and face are acquired from continual contraction of facial muscles, such as from smiling or squinting in bright light or against the wind. Facial lines become more strongly delineated as a person ages.
FIGURE 2.5 The four basic fingerprint patterns (a) arch, (b) whorl, (c) loop, and (d) combination
Dermis
The dermis is deeper and thicker than the epidermis (see fig.2.1). Elastic and collagenous fibers within the dermis are arranged in definite patterns, producing lines of tension in the skin and providing skin tone (fig.2.6).There are many more elastic fibers in the dermis of a young person than in an elderly one, and a decreasing number of elastic fibers is apparently associated with aging.The extensive network of blood vessels in the dermis provides nourishment to the living portion of the epidermis. The dermis also contains many sweat glands, oil-secreting glands, nerve endings, and hair follicles.
Layers of the Dermis
The dermis is composed of two layers. The upper layer, called the stratum papillarosum (papillary layer), is in contact with the epidermis and accounts for about one-fifth of the entire dermis (see fig. 2.2). Numerous projections, called papillae, extend from the upper portion of the dermis into the epidermis. Papillae form the base for the friction ridges on the fingers and toes. The deeper and thicker layer of the dermis is called the stratum reticularosum (reticular layer). Fibers within this layer are more dense and regularly arranged to form a tough, flexible meshwork. It is quite distensible, as is evident in pregnant women or obese individuals, but it can be stretched too far, causing “tearing” of the dermis. The repair of a strained dermal area leaves a white streak called a stretch mark, or linea albicans. Lineae albicantes are frequently found on the buttocks, thighs, abdomen, and breasts (fig. 2.7).
Innervation of the Skin
The dermis of the skin has extensive innervation (nerve supply). Specialized integumentary effectors consist of smooth muscles or glands within the dermis that respond to motor impulses transmitted from the central nervous system to the skin by autonomic nerve fibers. Several types of sensory receptors respond to various tactile (touch), pressure, temperature, tickle, or pain stimuli. Some are free nerve endings, some form a network around hair follicles, and some extend into the papillae of the dermis. Certain areas of the body, such as the palms, soles, lips, and external genitalia, have a greater concentration of sensory receptors and are therefore more sensitive to touch.
The dermis is deeper and thicker than the epidermis (see fig.2.1). Elastic and collagenous fibers within the dermis are arranged in definite patterns, producing lines of tension in the skin and providing skin tone (fig.2.6).There are many more elastic fibers in the dermis of a young person than in an elderly one, and a decreasing number of elastic fibers is apparently associated with aging.The extensive network of blood vessels in the dermis provides nourishment to the living portion of the epidermis. The dermis also contains many sweat glands, oil-secreting glands, nerve endings, and hair follicles.
Layers of the Dermis
The dermis is composed of two layers. The upper layer, called the stratum papillarosum (papillary layer), is in contact with the epidermis and accounts for about one-fifth of the entire dermis (see fig. 2.2). Numerous projections, called papillae, extend from the upper portion of the dermis into the epidermis. Papillae form the base for the friction ridges on the fingers and toes. The deeper and thicker layer of the dermis is called the stratum reticularosum (reticular layer). Fibers within this layer are more dense and regularly arranged to form a tough, flexible meshwork. It is quite distensible, as is evident in pregnant women or obese individuals, but it can be stretched too far, causing “tearing” of the dermis. The repair of a strained dermal area leaves a white streak called a stretch mark, or linea albicans. Lineae albicantes are frequently found on the buttocks, thighs, abdomen, and breasts (fig. 2.7).
Innervation of the Skin
The dermis of the skin has extensive innervation (nerve supply). Specialized integumentary effectors consist of smooth muscles or glands within the dermis that respond to motor impulses transmitted from the central nervous system to the skin by autonomic nerve fibers. Several types of sensory receptors respond to various tactile (touch), pressure, temperature, tickle, or pain stimuli. Some are free nerve endings, some form a network around hair follicles, and some extend into the papillae of the dermis. Certain areas of the body, such as the palms, soles, lips, and external genitalia, have a greater concentration of sensory receptors and are therefore more sensitive to touch.
Vascular Supply of the Skin
Blood vessels within the dermis supply nutrients to the mitotically active stratum basale of the epidermis and to the cellular structures of the dermis, such as glands and hair follicles. Dermal blood vessels play an important role in regulating body temperature and blood pressure. Autonomic vasoconstriction or vasodilation responses can either shunt the blood away from the superficial dermal arterioles or permit it to flow freely throughout dermal vessels. Fever or shock can be detected by the color and temperature of the skin. Blushing is the result of involuntary vasodilation of dermal blood vessels.
Hypodermis
The hypodermis, or subcutaneous tissue, is not actually a part of the skin, but it binds the dermis to underlying organs. The hypodermis is composed primarily of loose connective tissue and adipose cells interlaced with blood vessels (see fig. 2.1). Collagenous and elastic fibers reinforce the hypodermis-particularly on the palms and soles, where the skin is firmly attached to underlying structures. The amount of adipose tissue in the hypodermis varies with the region of the body and the sex, age, and nutritional state of the individual. Females generally have about an 8% thicker hypodermis than males. This layer functions to store lipids, insulate and cushion the body, and regulate temperature.
Blood vessels within the dermis supply nutrients to the mitotically active stratum basale of the epidermis and to the cellular structures of the dermis, such as glands and hair follicles. Dermal blood vessels play an important role in regulating body temperature and blood pressure. Autonomic vasoconstriction or vasodilation responses can either shunt the blood away from the superficial dermal arterioles or permit it to flow freely throughout dermal vessels. Fever or shock can be detected by the color and temperature of the skin. Blushing is the result of involuntary vasodilation of dermal blood vessels.
Hypodermis
The hypodermis, or subcutaneous tissue, is not actually a part of the skin, but it binds the dermis to underlying organs. The hypodermis is composed primarily of loose connective tissue and adipose cells interlaced with blood vessels (see fig. 2.1). Collagenous and elastic fibers reinforce the hypodermis-particularly on the palms and soles, where the skin is firmly attached to underlying structures. The amount of adipose tissue in the hypodermis varies with the region of the body and the sex, age, and nutritional state of the individual. Females generally have about an 8% thicker hypodermis than males. This layer functions to store lipids, insulate and cushion the body, and regulate temperature.

FIGURE 2.6 Lines of tension are caused by the pull of elastic and collagenous fibers within the dermis of the skin. Surgical incisions made parallel to the lines of tension heal more rapidly and create less scar tissue than those made across the lines of tension.
FIGURE 2.7 Stretch marks (lineae albicantes) on the abdomen of a pregnant woman. Stretch marks generally fade with time but may leave permanent markings.

Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!