Table 18.1 Nomenclature of bone tumors
Cardiac Tamponade
BASIC INFORMATION
DEFINITION
Cardiac tamponade is compression of the heart by fluid within the pericardial sac that impairs dilation and filling of the ventricles during diastole.
PHYSICAL FINDINGS & CLINICAL PRESENTATION
Acute cardiac tamponade (e.g., penetrating wounds, iatrogenic, aortic dissection)
1. Beck’s triad
a. Decrease in systemic arterial pressure
b. Elevated central venous pressure
c. Small, quiet heart
Chronic accumulating pericardial effusion leading to tamponade
1. Pericardial friction rub may be present
2. Tachypnea and tachycardia
3. Raised jugular venous distention (prominent x descent with absent y descent)
4. Pulsus paradoxus (>10 mm Hg fall in systolic blood pressure during inspiration)
5. Soft heart sounds

Figure 13. The top half of the figure represents the normal situation in which changes in intrathoracic pressure are transmitted to both the pericardial sac and the pulmonary veins. The effective filling gradient (EFG) changes only slightly during respiration. The bottom half of the figure represents cardiac tamponade in which changes in intrathoracic pressure are transmitted to the pulmonary veins but not to the pericardial sac. The EFG falls during inspiration. Insp, inspiration; LA, left atrium; LV, left ventricle; PC, pulmonary capillaries; PV, pulmonary veins.
ETIOLOGY
Acute
1. Penetrating trauma
2. Aortic dissection
3. Myocardial rupture after treatment of MI with thrombolytics and/or heparin
4. Iatrogenic (central line and pacemaker insertions, postcoronary bypass surgery)
Chronic accumulating pericardial effusion leading to tamponade
1. Malignancy (e.g., lung, breast, lymphoma)
2. Viral pericarditis (e.g., coxsackie, HIV)
3. Uremia
4. Bacterial, fungal, and tuberculosis
5. Myxedema (rare)
6. Collagen-vascular disease (e.g., SLE, RA, scleroderma)
7. Radiation
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
COPD, constrictive pericardial disease, restrictive cardiomyopathy, right ventricular infarction, and pulmonary embolism can all lead to elevated jugular venous pressure, decreased systemic pressure, and pulsus paradoxus.
WORKUP
Acute
1. Penetrating trauma
2. Aortic dissection
3. Myocardial rupture after treatment of MI with thrombolytics and/or heparin
4. Iatrogenic (central line and pacemaker insertions, postcoronary bypass surgery)
Chronic accumulating pericardial effusion leading to tamponade
1. Malignancy (e.g., lung, breast, lymphoma)
2. Viral pericarditis (e.g., coxsackie, HIV)
3. Uremia
4. Bacterial, fungal, and tuberculosis
5. Myxedema (rare)
6. Collagen-vascular disease (e.g., SLE, RA, scleroderma)
7. Radiation
DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
COPD, constrictive pericardial disease, restrictive cardiomyopathy, right ventricular infarction, and pulmonary embolism can all lead to elevated jugular venous pressure, decreased systemic pressure, and pulsus paradoxus.
WORKUP
Cardiac tamponade is a clinical diagnosis made at the bedside by noting the above-mentioned physical findings. The echocardiogram will support the clinical diagnosis. Thereafter, one must pursue the etiology with specific laboratory work (see below).
LABORATORY TESTS
• Electrolytes, BUN, Cr, ESR, thyroid function tests, ANA, RF, PPD, blood cultures, viral titers, and pericardial fluid analysis and cultures will all help in identifying or excluding a possible etiology of the effusion leading to tamponade.
• 12-lead ECG findings are suggestive but not diagnostic.
1. Low voltage (<5 mm QRS amplitude in the limb leads and <10 mm in the chest leads)
2. PR depression
3. Electrical alternans (alternating amplitude of the QRS complex in any or all leads)
IMAGING STUDIES
• The chest x-ray examination is not very specific. The heart size can be normal in acute tamponade or massive (water bottle configuration) in slow-forming effusions.
• The echocardiogram can detect effusions as small as 20 ml and can strongly suggest tamponade physiology (collapse of the right atrium and right ventricle during diastole).
• Right-sided cardiac catheterization and intrapericardial pressure measurements confirm the diagnosis.
• Typical findings are diastolic equalization of pressures (pulmonary artery pressure = right ventricular diastolic pressure = right atrial pressure = intrapericardial pressure).
LABORATORY TESTS
• Electrolytes, BUN, Cr, ESR, thyroid function tests, ANA, RF, PPD, blood cultures, viral titers, and pericardial fluid analysis and cultures will all help in identifying or excluding a possible etiology of the effusion leading to tamponade.
• 12-lead ECG findings are suggestive but not diagnostic.
1. Low voltage (<5 mm QRS amplitude in the limb leads and <10 mm in the chest leads)
2. PR depression
3. Electrical alternans (alternating amplitude of the QRS complex in any or all leads)
IMAGING STUDIES
• The chest x-ray examination is not very specific. The heart size can be normal in acute tamponade or massive (water bottle configuration) in slow-forming effusions.
• The echocardiogram can detect effusions as small as 20 ml and can strongly suggest tamponade physiology (collapse of the right atrium and right ventricle during diastole).
• Right-sided cardiac catheterization and intrapericardial pressure measurements confirm the diagnosis.
• Typical findings are diastolic equalization of pressures (pulmonary artery pressure = right ventricular diastolic pressure = right atrial pressure = intrapericardial pressure).
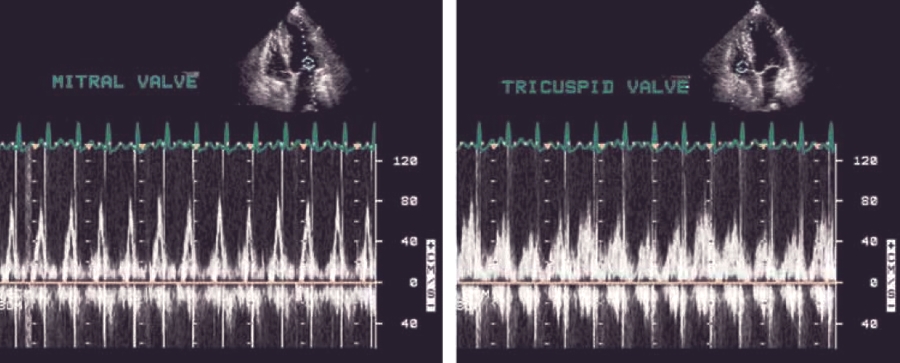
Fig. 14. Cardiac tamponade: ventricular filling.
TREATMENT
NONPHARMACOLOGIC THERAPY
Cardiac tamponade should be treated urgently. Avoid drugs that will reduce preload and exacerbate tamponade (e.g., nitrates, diuretics).
ACUTE GENERAL Rx
• The acute forms of tamponade as mentioned earlier (see “Etiology”) usually require emergency cardiothoracic surgery.
• Provide hemodynamic support with volume expansion and vasopressors along with emergency subxiphoid pericardiocentesis in the suspected tamponade code situation (e.g., electromechanical dissociation, patient in shock).
CHRONIC Rx
• Depends on etiology
• Semiacute treatment includes:
1. Right-side heart catheter with echocardiographic guided pericardiocentesis (can be done by cardiology). The catheter can be left in place for 48 hr to allow for continued drainage until a more definitive procedure is performed or the etiology is resolved (e.g., dialysis for uremia, levothyroxine for myxedema).
• Other surgical drainage procedures include:
1. Subxiphoid pericardial drainage
2. Limited pericardiectomy draining the pericardial fluid into the left hemithorax
3. Complete pericardiectomy
DISPOSITION
The prognosis of cardiac tamponade depends on the underlying cause.
NONPHARMACOLOGIC THERAPY
Cardiac tamponade should be treated urgently. Avoid drugs that will reduce preload and exacerbate tamponade (e.g., nitrates, diuretics).
ACUTE GENERAL Rx
• The acute forms of tamponade as mentioned earlier (see “Etiology”) usually require emergency cardiothoracic surgery.
• Provide hemodynamic support with volume expansion and vasopressors along with emergency subxiphoid pericardiocentesis in the suspected tamponade code situation (e.g., electromechanical dissociation, patient in shock).
CHRONIC Rx
• Depends on etiology
• Semiacute treatment includes:
1. Right-side heart catheter with echocardiographic guided pericardiocentesis (can be done by cardiology). The catheter can be left in place for 48 hr to allow for continued drainage until a more definitive procedure is performed or the etiology is resolved (e.g., dialysis for uremia, levothyroxine for myxedema).
• Other surgical drainage procedures include:
1. Subxiphoid pericardial drainage
2. Limited pericardiectomy draining the pericardial fluid into the left hemithorax
3. Complete pericardiectomy
DISPOSITION
The prognosis of cardiac tamponade depends on the underlying cause.

Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!