Accessory Organs of Digestion
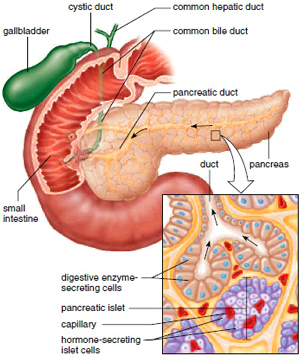
The salivary glands and even the teeth are accessory organs of digestion. The pancreas, liver, and gallbladder are also accessory digestive organs. Figure 15.10 shows how the pancreatic duct from the pancreas and the common bile duct from the liver and gallbladder join before entering the duodenum.
The Pancreas
The pancreas lies deep in the abdominal cavity, behind the peritoneum, resting on the posterior abdominal wall. Its broad end, called the head, more than fills the loop formed by the duodenum, and its tail extends in the opposite direction (Fig. 15.10). The pancreas has both an endocrine and an exocrine function. Pancreatic islets (islets of Langerhans) secrete insulin and glucagon, hormones that help keep the blood glucose level within normal limits. In this page, however, we are interested in the exocrine function of the pancreas. Most pancreatic cells, called pancreatic acinar cells, produce pancreatic juice, which is secreted into tiny tubes that unite, forming ever-larger ones. Finally, a single pancreatic duct extends the length of the pancreas to the duodenum.
Pancreatic Juice
Pancreatic juice contains sodium bicarbonate (NaHCO3) and digestive enzymes for all types of food. Sodium bicarbonate neutralizes chyme; whereas pepsin acts best in an acid pH of the stomach, pancreatic enzymes require a slightly basic pH. Pancreatic amylase digests starch, trypsin digests protein, and lipase digests fat. Pancreatic juice also contains two nucleases, which are enzymes that break down nucleic acid molecules into nucleotides. In cystic fibrosis, a thick mucus blocks the pancreatic duct, and the patient must take supplemental pancreatic enzymes by mouth for proper digestion to occur.
The Liver
The liver, which is the largest organ in the body, lies mainly in the upper right section of the abdominal cavity, just inferior to the diaphragm (see Fig. 15.1).
Liver Structure
The liver has two main lobes, the right lobe and the smaller left lobe, separated by a ligament. Each lobe is divided into many hepatic lobules that serve as its structural and functional units (Fig. 15.11). A lobule consists of many hepatic cells arranged in longitudinal groups that radiate out from a central vein. Hepatic sinusoids separate the groups of cells from each other. Large fixed phagocytic cells called Kupffer cells are attached to the lining of the hepatic sinusoids. They remove pathogens and debris that may have entered the hepatic portal vein at the small intestine.
Pancreatic juice contains sodium bicarbonate (NaHCO3) and digestive enzymes for all types of food. Sodium bicarbonate neutralizes chyme; whereas pepsin acts best in an acid pH of the stomach, pancreatic enzymes require a slightly basic pH. Pancreatic amylase digests starch, trypsin digests protein, and lipase digests fat. Pancreatic juice also contains two nucleases, which are enzymes that break down nucleic acid molecules into nucleotides. In cystic fibrosis, a thick mucus blocks the pancreatic duct, and the patient must take supplemental pancreatic enzymes by mouth for proper digestion to occur.
The Liver
The liver, which is the largest organ in the body, lies mainly in the upper right section of the abdominal cavity, just inferior to the diaphragm (see Fig. 15.1).
Liver Structure
The liver has two main lobes, the right lobe and the smaller left lobe, separated by a ligament. Each lobe is divided into many hepatic lobules that serve as its structural and functional units (Fig. 15.11). A lobule consists of many hepatic cells arranged in longitudinal groups that radiate out from a central vein. Hepatic sinusoids separate the groups of cells from each other. Large fixed phagocytic cells called Kupffer cells are attached to the lining of the hepatic sinusoids. They remove pathogens and debris that may have entered the hepatic portal vein at the small intestine.
Portal triads consisting of the following three structures are located between the lobules: a bile duct that takes bile away from the liver; a branch of the hepatic artery that brings O2-rich blood to the liver; and a branch of the hepatic portal vein that transports nutrients from the intestines. The bile ducts merge to form the common hepatic duct. The central veins of the lobules enter a hepatic vein. With the help of Figure 12.20, trace the path of blood from the intestines to the liver via the hepatic portal vein and from the liver to the inferior vena cava via the hepatic veins.
Figure 15.10 The pancreas is an exocrine gland when it secretes digestive enzymes into tubes that join to become the pancreatic duct. The pancreatic duct and the common bile duct empty into the duodenum of the small intestine. Pancreatic juice contains enzymes that digest all types of food: carbohydrates, fats, proteins, and nucleic acids.
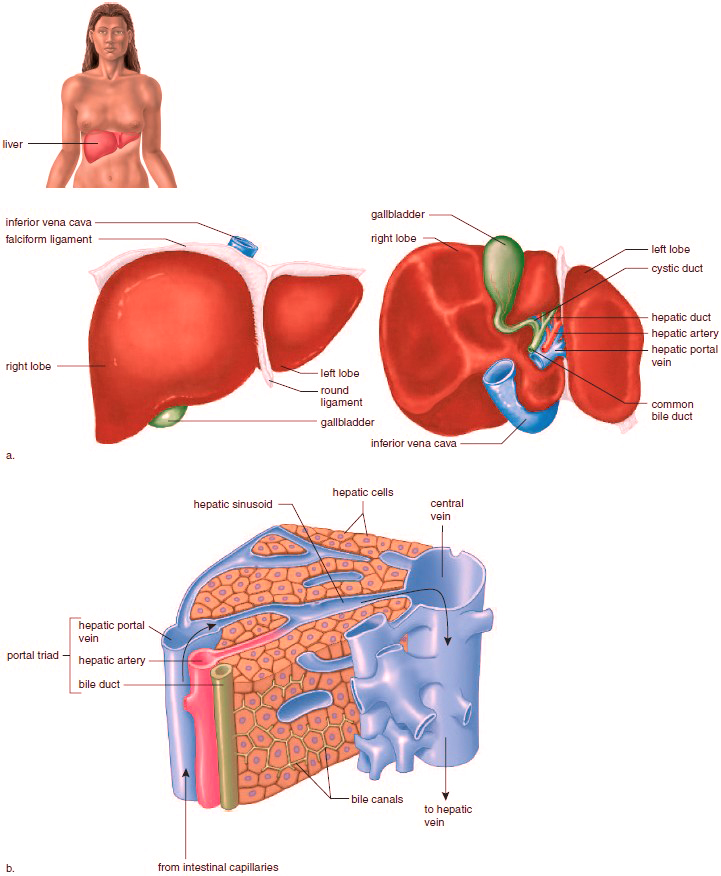
Figure 15.11 Macroscopic and microscopic anatomy of the liver. a. The liver has two lobes viewed anteriorly (left) and posteriorly (right). b. Cross section of a hepatic lobule, illustrating microscopic structure.
Liver Functions
As the blood from the hepatic portal vein passes through the liver, hepatic cells remove poisonous substances and detoxify them. The liver also removes nutrients and works to keep the contents of the blood constant. It removes and stores iron and the fat-soluble vitamins A, D, E, and K; makes the plasma proteins from amino acids; and helps regulate the quantity of cholesterol in the blood. The liver maintains the blood glucose level at about 100 mg/100 ml (0.1%), even though a person eats intermittently. When insulin is present, any excess glucose in the blood is removed and stored by the liver as glycogen. Between meals, glycogen is broken down to glucose, which enters the hepatic veins, and in this way, the blood glucose level remains constant. If the supply of glycogen is depleted, the liver converts glycerol (from fats) and amino acids to glucose molecules. The conversion of amino acids to glucose necessitates deamination, the removal of amino groups and the production of ammonia. By a complex metabolic pathway, the liver then combines ammonia with carbon dioxide to form urea:
As the blood from the hepatic portal vein passes through the liver, hepatic cells remove poisonous substances and detoxify them. The liver also removes nutrients and works to keep the contents of the blood constant. It removes and stores iron and the fat-soluble vitamins A, D, E, and K; makes the plasma proteins from amino acids; and helps regulate the quantity of cholesterol in the blood. The liver maintains the blood glucose level at about 100 mg/100 ml (0.1%), even though a person eats intermittently. When insulin is present, any excess glucose in the blood is removed and stored by the liver as glycogen. Between meals, glycogen is broken down to glucose, which enters the hepatic veins, and in this way, the blood glucose level remains constant. If the supply of glycogen is depleted, the liver converts glycerol (from fats) and amino acids to glucose molecules. The conversion of amino acids to glucose necessitates deamination, the removal of amino groups and the production of ammonia. By a complex metabolic pathway, the liver then combines ammonia with carbon dioxide to form urea:

Urea is the usual nitrogenous waste product from amino acid breakdown in humans. After its formation in the liver, urea is excreted by the kidneys. The liver produces bile, which is stored in the gallbladder. Bile has a yellowish-green color because it contains the bile pigment bilirubin, which is derived from the breakdown of hemoglobin, the red pigment of red blood cells. Bile also contains bile salts.
Bile salts are derived from cholesterol, and they emulsify fat in the small intestine. When fat is emulsified, it breaks up into droplets, providing a much larger surface area, which can be acted upon by a digestive enzyme from the pancreas. Altogether, the following are significant ways in which the liver helps maintain homeostasis:
1. Detoxifies blood by removing and metabolizing poisonous substances.
2. Stores iron (Fe2+) and the fat-soluble vitamins A, D, E, and K.
3. Makes plasma proteins, such as albumins and fibrinogen, from amino acids.
4. Stores glucose as glycogen after a meal, and breaks down glycogen to glucose to maintain the glucose concentration of blood between eating periods.
5. Produces urea after breaking down amino acids.
6. Destroys old red blood cells; excretes bilirubin, a breakdown product of hemoglobin in bile, a liver product.
7. Helps regulate the blood cholesterol level, converting some to bile salts.
Liver Disorders
When a person has a liver ailment, jaundice may occur. Jaundice is a yellowish tint to the whites of the eyes and also to the skin of light-pigmented persons. Bilirubin is deposited in the skin due to an abnormally large amount in the blood. In hemolytic jaundice, red blood cells have been broken down in abnormally large amounts; in obstructive jaundice, bile ducts are blocked, or liver cells are damaged. Jaundice can also result from hepatitis, inflammation of the liver. Viral hepatitis occurs in several forms. Hepatitis A is usually acquired from sewage-contaminated drinking water. Hepatitis B, which is usually spread by sexual contact, can also be spread by blood transfusions or contaminated needles. The hepatitis B virus is more contagious than the AIDS virus, which is spread in the same way. Thankfully, however, a vaccine is now available for hepatitis B. Hepatitis C, which is usually acquired by contact with infected blood and for which there is no vaccine, can lead to chronic hepatitis, liver cancer, and death.
Cirrhosis is another chronic disease of the liver. First the organ becomes fatty, and then liver tissue is replaced by inactive fibrous scar tissue. Cirrhosis of the liver is often seen in alcoholics due to malnutrition and the excessive amounts of alcohol (a toxin) the liver is forced to break down. Hepatitis and cirrhosis affect the entire liver and hinder its ability to repair itself. Therefore, they are life-threatening diseases. The liver has amazing regenerative powers and can recover if the rate of regeneration exceeds the rate of damage. During liver failure, however, there may not be enough time to let the liver heal itself. Liver transplantation is usually the preferred treatment for liver failure, but artificial livers have been developed and tried in a few cases. One type is a cartridge that contains liver cells. The patient’s blood passes through the cellulose acetate tubing of the cartridge and is serviced in the same manner as with a normal liver. In the meantime, the patient’s liver has a chance to recover.
The Gallbladder
The gallbladder is a pear-shaped, muscular sac located in a depression on the inferior surface of the liver (see Fig. 15.11a). About 1,000 ml of bile are produced by the liver each day, and any excess is stored in the gallbladder. Water is reabsorbed by the gallbladder so that bile becomes a thick, mucuslike material. When needed, bile leaves the gallbladder by way of the cystic duct. The cystic duct and the common hepatic duct join to form the common bile duct, which enters the duodenum. The cholesterol content of bile can come out of solution and form crystals. If the crystals grow in size, they form gallstones. The passage of the stones from the gallbladder may block the common bile duct and cause obstructive jaundice. Then the gallbladder may have to be removed.
Function of Bile Salts
Bile salts carry out emulsification; they break up masses of fat into droplets that can be acted on by enzymes that digest fat. Through their ability to make fats interact with water, they also enhance absorption of fatty acids, cholesterol, and the fat-soluble vitamins A, D, E, and K.
1. Detoxifies blood by removing and metabolizing poisonous substances.
2. Stores iron (Fe2+) and the fat-soluble vitamins A, D, E, and K.
3. Makes plasma proteins, such as albumins and fibrinogen, from amino acids.
4. Stores glucose as glycogen after a meal, and breaks down glycogen to glucose to maintain the glucose concentration of blood between eating periods.
5. Produces urea after breaking down amino acids.
6. Destroys old red blood cells; excretes bilirubin, a breakdown product of hemoglobin in bile, a liver product.
7. Helps regulate the blood cholesterol level, converting some to bile salts.
Liver Disorders
When a person has a liver ailment, jaundice may occur. Jaundice is a yellowish tint to the whites of the eyes and also to the skin of light-pigmented persons. Bilirubin is deposited in the skin due to an abnormally large amount in the blood. In hemolytic jaundice, red blood cells have been broken down in abnormally large amounts; in obstructive jaundice, bile ducts are blocked, or liver cells are damaged. Jaundice can also result from hepatitis, inflammation of the liver. Viral hepatitis occurs in several forms. Hepatitis A is usually acquired from sewage-contaminated drinking water. Hepatitis B, which is usually spread by sexual contact, can also be spread by blood transfusions or contaminated needles. The hepatitis B virus is more contagious than the AIDS virus, which is spread in the same way. Thankfully, however, a vaccine is now available for hepatitis B. Hepatitis C, which is usually acquired by contact with infected blood and for which there is no vaccine, can lead to chronic hepatitis, liver cancer, and death.
Cirrhosis is another chronic disease of the liver. First the organ becomes fatty, and then liver tissue is replaced by inactive fibrous scar tissue. Cirrhosis of the liver is often seen in alcoholics due to malnutrition and the excessive amounts of alcohol (a toxin) the liver is forced to break down. Hepatitis and cirrhosis affect the entire liver and hinder its ability to repair itself. Therefore, they are life-threatening diseases. The liver has amazing regenerative powers and can recover if the rate of regeneration exceeds the rate of damage. During liver failure, however, there may not be enough time to let the liver heal itself. Liver transplantation is usually the preferred treatment for liver failure, but artificial livers have been developed and tried in a few cases. One type is a cartridge that contains liver cells. The patient’s blood passes through the cellulose acetate tubing of the cartridge and is serviced in the same manner as with a normal liver. In the meantime, the patient’s liver has a chance to recover.
The Gallbladder
The gallbladder is a pear-shaped, muscular sac located in a depression on the inferior surface of the liver (see Fig. 15.11a). About 1,000 ml of bile are produced by the liver each day, and any excess is stored in the gallbladder. Water is reabsorbed by the gallbladder so that bile becomes a thick, mucuslike material. When needed, bile leaves the gallbladder by way of the cystic duct. The cystic duct and the common hepatic duct join to form the common bile duct, which enters the duodenum. The cholesterol content of bile can come out of solution and form crystals. If the crystals grow in size, they form gallstones. The passage of the stones from the gallbladder may block the common bile duct and cause obstructive jaundice. Then the gallbladder may have to be removed.
Function of Bile Salts
Bile salts carry out emulsification; they break up masses of fat into droplets that can be acted on by enzymes that digest fat. Through their ability to make fats interact with water, they also enhance absorption of fatty acids, cholesterol, and the fat-soluble vitamins A, D, E, and K.
Contacts: lubopitno_bg@abv.bg www.encyclopedia.lubopitko-bg.com Corporation. All rights reserved.
DON'T FORGET - KNOWLEDGE IS EVERYTHING!